Chandramohan Meenakshisundaram, MD
Nanditha Malakkla, MD
Saint Francis Hospital
Evanston, IL

Figure 1. Admission chest x-ray showing hyper-aerated lung fields and consolidation at the left lung base.
Figure 2. Video of selected images from thoracic CT scan in soft tissue windows showing large mediastinal mass with extravasation of contrast.
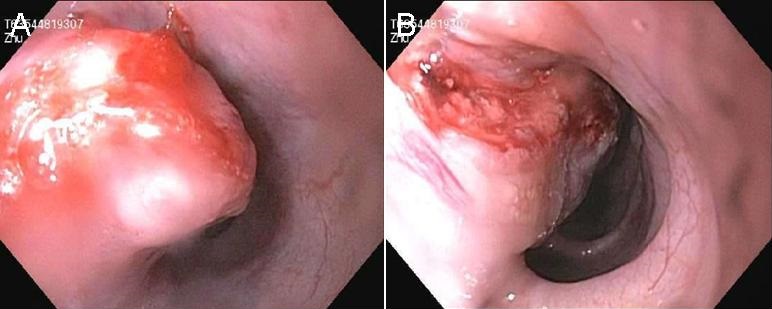
Figure 3. Views from endoscopy showing a large mass and the perforation site.
A 66-year-old Asian man with no significant past medical history was admitted with 1 week history of worsening retrosternal sharp chest pain, dyspnea on moderate exertion, and cough productive of brownish sputum. He also complained of some difficulty swallowing, decreased appetite and weight loss for the past 3 months. PPD was negative in the past. Vitals signs were significant for tachycardia and low grade fever. On physical exam he was cachectic and lung auscultation revealed bilateral scattered wheezes. Basic labs including complete blood count and comprehensive metabolic panel were unremarkable. EKG showed sinus tachycardia, serial troponin I was negative and chest x-ray revealed bilateral hyper-aerated lung fields and consolidation over the left lung base (Figure 1). He was started on antibiotics and bronchodilators. Since he continued to have chest pain and remained tachycardic, CT angiography of chest and abdomen (with IV and oral contrast) was done which revealed extravasation of contrast material into the mediastinum in the mid esophageal region representing rupture, a large mediastinal mass concerning for an abscess, and extensive infiltrates in the left lower lobe (Figure 2). During left thoracotomy, a large amount of necrotic material and phlegmon was seen in the mediastinum with adjacent area of lung necrosis which was drained and debrided. Upper GI endoscopy revealed a large mass in the mid-esophagus with perforation for which stenting was done (Figure 3). Pathology of phlegmon revealed squamous cell carcinoma with extensive necrosis. Culture of the fluid grew both viridians streptococci and anaerobes and he was started on broad spectrum antibiotics. His post-operative course was complicated and later he elected hospice care.
Reference as: Meenakshisundaram C, Malakkla N. Medical image of the week: eosphageal cancer. Southwest J Pulm Crit Care. 2014;9(5):295-6. doi: http://dx.doi.org/10.13175/swjpcc151-14 PDF