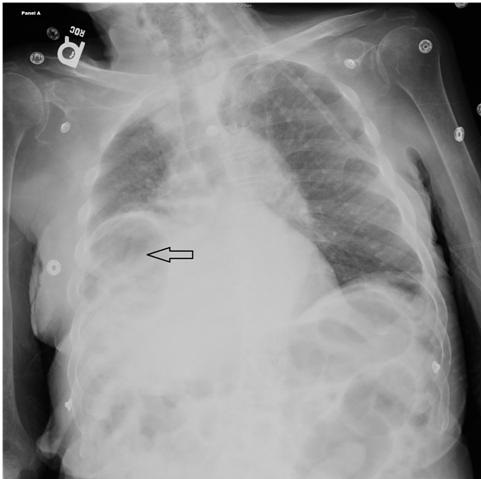
Figure 1. An X-ray of the chest showing a lucency under the right hemi-diaphragm interposed between the liver and diaphragm (arrow).
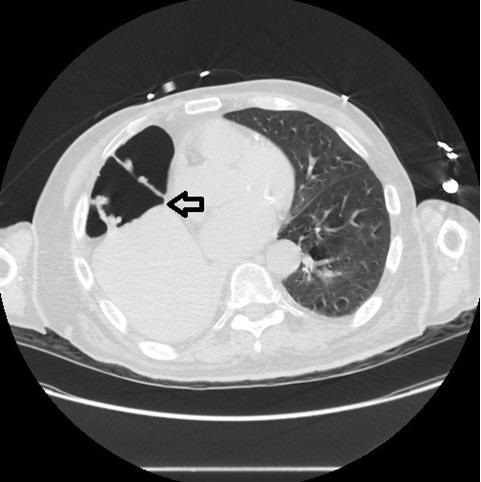
Figure 2. CT scan of the chest showing gas filled distended hepatic flexure interposed between the elevated right hemi-diaphragm and the liver (arrow).
X-ray evidence of air under right hemi-diaphragm in proper clinical context is almost a definitive sign of gastrointestinal tract perforation except in an extremely rare clinical entity called "Chilaiditi Syndrome". We present this unique image and clinical scenario to expand on physician`s knowledge to identify this rare clinical syndrome and to help distinguish it from a dreaded condition like gastrointestinal perforation.
An 81-year-old man with multiple co-morbidities was admitted to the intensive care unit with a diagnosis of acute hypoxic respiratory failure. An X-ray of the chest showed a lucency under the right hemi-diaphragm interposed between the liver and diaphragm (Figure 1). Due to radiological concern of gastrointestinal perforation, an emergent CT scan was performed to rule out perforation. CT scan revealed gas filled distended hepatic flexure interposed between the elevated right hemi-diaphragm and the liver (Figure 2). The patient had no gastro-intestinal tract symptoms and no pathological signs were specifically identified on clinical examination; a diagnosis of the Chilaiditi Syndrome was made. Chilaiditi Syndrome occurs due to interposition of a loop of large intestine in between the liver and the diaphragm. The incidence of Chilaiditi Syndrome is 0.025 to 0.28% and occurs because of congenital anatomical variations of falciform ligament (1). It can also be due to functional abnormalities such as constipation, aerophagia, cirrhosis, paralysis of the diaphragm, chronic lung disease which can cause enlargement of the lower thoracic cavity, obesity, and processes which increase intra-abdominal pressure (1,2). Initial management includes conservative therapy - Bed rest, intravenous fluid hydration, and bowel decompression. Surgical options can be considered (3).
Priyanka Makkar, M.D.1, Rishabh Mishra, M.D.1, and Shivanck Upadhyay, M.D.2
1Internal Medicine department, St. Barnabas Hospital, Bronx, New York
2Department of Pulmonary Critical Care Medicine, St. Barnabas Hospital, Bronx, New York
References
- Alva S, Shetty-Alva N, Longo WE. Image of the month. Chilaiditi sign or syndrome. Arch Surg. 2008 Jan;143(1):93-4. [CrossRef] [PubMed]
- Fisher AA, Davis MW. An elderly man with chest pain, shortness of breath, and constipation. Postgrad Med J. 2003 Mar;79(929):180, 183-4. [CrossRef] [PubMed]
- Blevins WA, Cafasso DE, Fernandez M, Edwards MJ.Minimally invasive colopexy for pediatric Chilaiditi syndrome. J Pediatr Surg. 2011 Mar;46(3):e33-5. [CrossRef] [PubMed]
Cite as: Makkar P, Mishra R, Upadhyay S. Medical image of the week: Chilaiditi syndrome. Southwest J Pulm Crit Care. 2016;13(4):179-80. doi: http://dx.doi.org/10.13175/swjpcc077-16 PDF