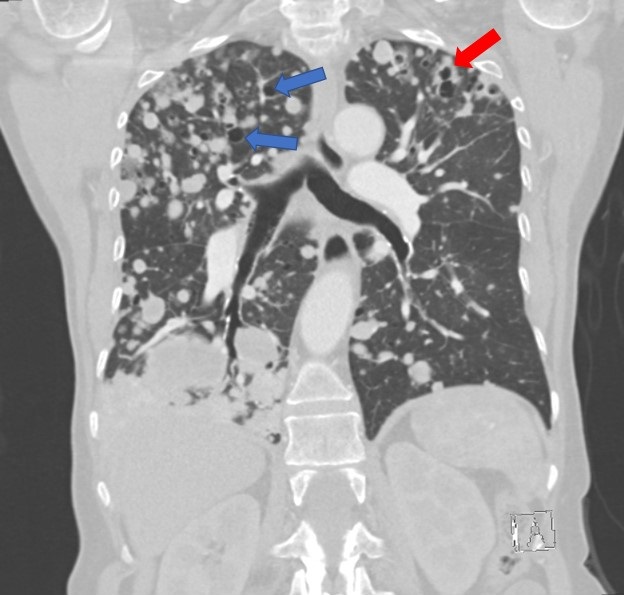
Figure 1. A coronal reconstruction of the patient’s CT of the chest with contrast in lung windows demonstrates extensive, bilateral metastatic disease, with the greatest burden of disease situated in the right lower lobe. Areas of cystic change (blue arrows) and cavitary disease (red arrow) are present.
Clinical Scenario: A 71-year-old woman with primary malignancy of the breast in remission post bilateral mastectomy in 2005 and 2008, presented to the emergency room with progressive shortness of breath for the past 6 months. Upon arrival to the emergency room, she described localized sharp chest pain along the right thoracic wall which had gradually worsened over the past three months. The pain was exacerbated with movement and with deep inspiration. She also endorsed significant hemoptysis, expectorating approximately 500 ml of bloody sputum on the morning of her presentation. Pertinent vitals revealed that she was both tachycardic and tachypneic, saturating 94% on room air with an increased work of breathing. Physical examination was significant for coarse breath sounds and diminished right sided lung sounds. Initial labs demonstrated a normal troponin and an unremarkable EKG. A chest radiograph demonstrated a large left mediastinal and hilar mass with numerous parenchymal nodules bilaterally. A CT of the chest with contrast (Figure 1) demonstrated widespread lung nodules, most notably in the right lung with a confluent mass in the right base. No significant focal lesions were seen in the chest wall or breast regions. A biopsy of the left mediastinal mass was performed and confirmed metastatic spindle cell carcinoma originating from her primary breast cancer.
Discussion: Spindle cell carcinoma of the breast, a variant classified under metaplastic carcinoma, is a rare entity occurring in less than 1% of all incidences of primary breast cancer, and most commonly seen in postmenopausal women (2,5). Treatment is primarily surgical resection. The role of radiation and chemotherapy is unclear and varies per patient treatment plan. Tumors are typically triple-negative, limiting therapeutic options (1,2,5). Primary tumor diameter and grade may be the most important prognostic factors, although prognosis regarding spindle cell carcinoma is generally poor. At the time of diagnosis, incidence of axillary lymph node metastasis was 40 – 56% with a high grade of recurrence at 57% - 63% (1,4,5). Most common extra nodal metastasis was to the lungs. In addition to the poor prognosis of spindle cell carcinomas and high rates of local recurrence, metastatic disease is also frequently seeing in patients, such as the metastatic disease seen with our patient (2-4).
Our patient’s primary breast cancer was treated with a bilateral mastectomy followed by neither chemotherapy nor radiation therapy based on patient’s preference and discussion with her oncology team. The primary tumor was in the left breast with recurrence to the right breast and metastasis to bilateral lungs. Like other cases, a biopsy revealed a triple-negative tumor. She was discharged on supplemental oxygen and is expected to receive P13K inhibitor therapy for targeted palliative treatment.
Vinita Kusupati MD, MBA and Stefano Natali DO
Department of Internal Medicine,
Banner University Medical Center-Tucson Campus
Tucson, AZ USA
References
- Adem C, Reynolds C, Ingle JN, Nascimento AG. Primary breast sarcoma: clinicopathologic series from the Mayo Clinic and review of the literature. Br J Cancer. 2004 Jul 19;91(2):237-41. [CrossRef] [PubMed]
- Alaoui M'hamdi H, Abbad F, Rais H, Asmouki H, Soumani A, Khouchani M, Belbaraka R. Rare variant of metaplastic carcinoma of the breast: a case report and review of the literature. J Med Case Rep. 2018 Feb 21;12(1):43. [CrossRef] [PubMed]
- Carter MR, Hornick JL, Lester S, Fletcher CD. Spindle cell (sarcomatoid) carcinoma of the breast: a clinicopathologic and immunohistochemical analysis of 29 cases. Am J Surg Pathol. 2006 Mar;30(3):300-9. [CrossRef] [PubMed]
- Khan HN, Wyld L, Dunne B, Lee AH, Pinder SE, Evans AJ, Robertson JF. Spindle cell carcinoma of the breast: a case series of a rare histological subtype. Eur J Surg Oncol. 2003 Sep;29(7):600-3. [CrossRef] [PubMed]
- Tse GM, Tan PH, Putti TC, Lui PC, Chaiwun B, Law BK. Metaplastic carcinoma of the breast: a clinicopathological review. J Clin Pathol. 2006 Oct;59(10):1079-83. [CrossRef] [PubMed]
- Tse GM, Tan PH, Lui PC, Putti TC. Spindle cell lesions of the breast--the pathologic differential diagnosis. Breast Cancer Res Treat. 2008 May;109(2):199-207. [CrossRef] [PubMed]
Cite as: Kusupati V, Natali S. Medical image of the month: metastatic spindle cell carcinoma of the breast. Southwest J Pulm Crit Care. 2021;22(6):114-5. doi: https://doi.org/10.13175/swjpcc021-21 PDF