Griffin MR, Zhu Y, Moore MR, Whitney CG, Grijalva CG. U.S. hospitalizations for pneumonia after a decade of pneumococcal vaccination. N Engl J Med. 2013;369(2):155-63. [CrossRef] [PubMed]
The introduction of the 7-valent pneumococcal conjugate vaccine (PCV7) into the U.S. childhood immunization schedule in 2000 has substantially reduced the incidence of vaccine-serotype invasive pneumococcal disease in young children and in unvaccinated older children and adults. By preventing the acquisition and carriage of pneumococcus in the nasopharynx of vaccinated children, PCV7 reduced the transmission of vaccine serotypes to the unvaccinated. The authors estimated the annual rates of hospitalization for pneumonia from any cause using the Nationwide Inpatient Sample database. Average annual rates of pneumonia-related hospitalizations from 1997 through 1999 (before the introduction of PCV7) and from 2007 through 2009 (well after its introduction) were used to estimate annual declines in hospitalizations due to pneumonia. The annual rate of hospitalization for pneumonia among children younger than 2 years of age declined by 551.1 per 100,000 children. The rate for adults 85 years of age or older also declined by 1300.8 per 100,000. Overall, the authors estimated an age-adjusted annual reduction of 54.8 per 100,000, or 168,000 fewer hospitalizations for pneumonia annually.
Taken at face value this article would appear to provide convincing evidence of the efficacy of PCV7. However, the same argument was made for the 23-polyvalent pneumococcal vaccine (PPV-23) in adults. Beginning in the mid-1990’s the Veterans Administration (VA) made a large effort to increase the rates of pneumococcal vaccination which was quite successful (Figure 1) (1).
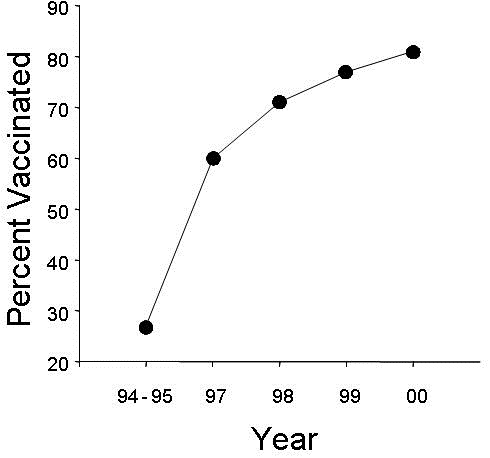
Figure 1. Percent of VA patients vaccinated with PPV-23 by year (1).
The VA touted this increase in vaccination as responsible for a decrease in inpatient admissions for pneumonia (Figure 2) (2).
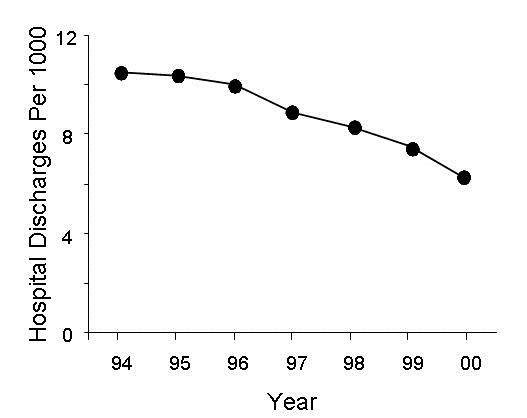
Figure 2. Hospital discharges per 1000 for pneumonia by year (2).
However, what was not cited was that hospital discharges for all groups were decreasing. Furthermore, there was an increase in outpatient visits for pneumonia (Figure 3) (3).
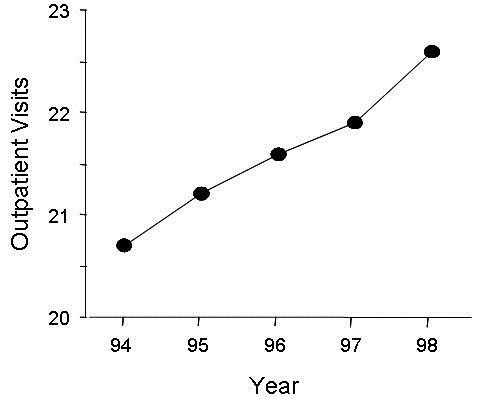
Figure 3. Risk-adjusted rates of clinic use in patients with pneumonia in the Veterans Administration 1994 through 1998 (3).
An increase in risk-adjusted one year survival occurred for pneumonia from 1994 through 1998 which was less than 1% (p=0.02) (3). However, the improvement in survival did not correlate with the increase in pneumococcal vaccination (r=0.19, p>0.05). Most of the improvement in survival occurred between 1994 and 1995 before the dramatic increase in PPV-23 vaccination rate occurred between 1995 and 1997. It would appear that the reduction in hospital admissions was part of a trend to increase outpatient therapy. There appeared to be no clinically significant impact on the incidence or mortality.
Determinants of hospitalization for pneumonia are many as the above illustrates. Since the introduction of PCV7 in 2000, there has been a 60% increase in the vaccination of adults 65 years of age or older with pneumococcal polysaccharide vaccine and an increase of 67% in influenza (4). During this same period, the percentage of adults who smoked fell to 24% (5). There has been increasing emphasis placed on outpatient therapy for pneumonia with assessment tools such as the pneumonia severity index and CURB-65 (6).
Despite the similarity of arguments for a decline in hospitalizations from PCV7, there is an important difference. There is strong evidence that PCV7 works in children while the efficacy of PPV-23 in adults is suspect (7,8). There is considerable year-to-year variability in the incidence of pneumonia with <5% actually diagnosed with pneumococcal disease (1). The influence of these and other factors such as influenza vaccine and variability in hospital admissions further confuse the issue (9). It may be that the authors are correct, that PCV7 does prevent pneumonia in adults. However, presenting only the hospital admission rates without accounting for at least some of the many confounding variables makes the overall level of evidence cited in this article unconvincing.
Richard A. Robbins, MD
References
- Jha AK, Perlin JB, Kizer KW, Dudley RA. Effect of the transformation of the Veterans Affairs Health Care System on the quality of care. N Engl J Med. 2003;348(22):2218-27. [CrossRef] [PubMed]
- Jha AK, Wright SM, Perlin JB. Performance measures, vaccinations, and pneumonia rates among high-risk patients in Veterans Administration health care. Am J Public Health. 2007;97(12):2167-72. [CrossRef] [PubMed]
- Ashton CM, Souchek J, Petersen NJ, et al. Hospital use and survival among Veterans Affairs beneficiaries. N Engl J Med. 2003;349(17):1637-1646. [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Seasonal influenza (flu): vaccination trends. Available at: http://www.cdc.gov/flu/fluvaxview/trends.htm (accessed 8/30/13).
- U.S. smoking rate still coming down. Gallup. July 24, 2008. Available at : http://www.gallup.com/poll/109048/us-smoking-rate-stillcoming-down.aspx (accessed 8/30/13).
- Varshochi M, Kianmehr P, Naghavi-Behzad M, Bayat-Makoo Z. Correspondence between hospital admission and the pneumonia severity index (PSI), CURB-65 criteria and comparison of their predictive value in mortality and hospital stay. Infez Med. 2013;21(2):103-10. [PubMed]
- Black SB, Shinefield HR, Ling S, Hansen J, Fireman B, Spring D, Noyes J, Lewis E, Ray P, Lee J, Hackell J. Effectiveness of heptavalent pneumococcal conjugate vaccine in children younger than five years of age for prevention of pneumonia. Pediatr Infect Dis J. 2002;21(9):810-5. [CrossRef] [PubMed]
- Huss A, Scott P, Stuck AE, Trotter C, Egger M. Efficacy of pneumococcal vaccination in adults: a meta-analysis. CMAJ. 2009;180(1):48-58. [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Comparability between the rates for all-listed inpatient procedures using national hospital discharge survey and Medicare claims, 1999 and 2007. September 27, 2012. Available at: http://www.cdc.gov/nchs/data/nhsr/nhsr057.pdf (accessed 8/30/13).
Reference as: Robbins RA. August 2013 pulmonary journal club: pneumococcal vaccine déjà vu. Southwest J Pulm Crit Care. 2013;7(2):131-4. doi: http://dx.doi.org/10.13175/swjpcc115-13 PDF