Bridgett Ronan, MD
Robert Viggiano, MD
Lewis J. Wesselius, MD
Pulmonary Medicine
Mayo Clinic Arizona
Scottsdale, AZ
History of Present Illness
A 63 year old man was transferred from outside facility with ventricular tachycardia. He has a past history of ventricular tachycardia and had an intracardiac defibrillator (ICD) placed due to a low ejection fraction. The ICD had administered several shocks to the patient prior to admission.
His present medications included:
- Lisinopril 10 mg bid
- Diazepam 10 mg bid
- Amiodarone 400 mg daily
- Dutasteride 0.5 mg daily
- Tamsulosin 0.4 mg daily
- Dexlansoprazole 60 mg daily
- Levothyroxine 100 mcg daily
The patient underwent and electrophysiology (EP) procedure. He was intubated prior to the procedure. He developed sustained ventricular tachycardia when the ICD was turned off. Eleven cardioversions were required with an accumulated 108 seconds of ventricular tachycardia. He became hypotensive and received 6.2 L boluses of fluids and 5, 400 mg boluses of amiodarone and was placed on an amiodarone drip.
He remained intubated receiving mechanical ventilator after the EP procedure.
He was extubated after 2 days and was initially on oxygen at 6L/min nasal cannula. Over the next several days he developed increasing oxygen requirements and was treated with BiPAP and increasing oxygen.
PMH, SH and FH
As noted above he had a history of recurrent ventricular tachycardia and a dilated cardiomyopathy with an ejection fraction of 30-35%. In addition he had a history of paroxysmal atrial fibrillation, obstructive sleep apnea which resolved with weight loss, hypothyroidism and mild restriction on pulmonary function testing, possibly related to amiodarone or to kyphosis. He is a life-long nonsmoker.
Physical Examination
His vital signs included a Tmax of 38.8 C, heart rate of 79 beats/min, blood pressure of 113/67 mm Hg, respiratory rate of 38 breaths/min, and oxygen saturation of 94% on a 75% high flow mask. His weight had increased to 102 kg from 96.6 kg on admission.
Cardiovascular exam revealed an irregular rhythm but no murmur. There was jugular venous distention present. There was a trace of pedal edema but deeper pitting edema at the hips.
Pulmonary auscultation revealed bilateral rales with diminished breath sounds at the bases.
Chest X-ray
Admission and current chest x-ray are shown in Figure 1.
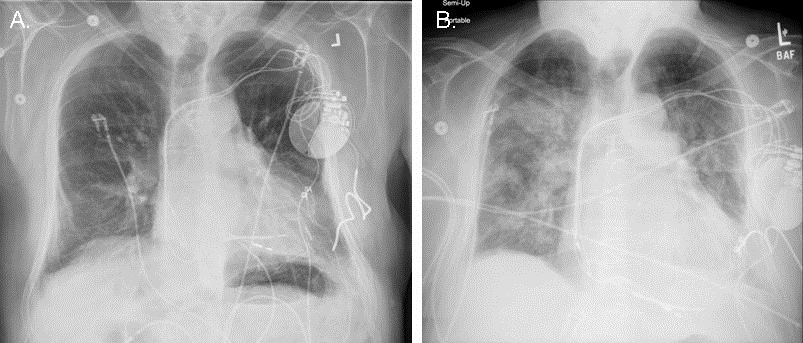
Figure 1. Admission chest x-ray (panel A) and current chest x-ray (panel B).
Laboratory Evaluation
Arterial blood gases showed a pH of 7.42, a pCO2 of 39 and a pO2 of 73 on 70% FiO2. The white blood cell count (WBC) was elevated at 15.1X103 cells/mm3.
Which of the following could explain the patient’s increased oxygen requirements?
Reference as: Ronan B, Viggiano R, Wesselius LJ. July 2012 pulmonary case of the month: pulmonary infiltrates - getting to the heart of the problem. Southwest J Pulm Crit Care 2012;5:1-11. (click here for a PDF version of the case)