Kelly Cawcutt, MD
Pritish Tosh, MD
Jennifer Elmer, RN, CNS
Scott Copeman, RRT
Christina Rivera, Pharm D, RPh
Division of Critical Care
Mayo Clinic
Rochester, Minnesota
History of Present Illness
A 58 year old woman, former smoker, presented to the pulmonary outpatient clinic at Mayo Clinic Rochester with dyspnea on exertion. In clinic, she was found to be tachycardic and febrile, and therefore, she was directly admitted to a medicine ward for possible sepsis.
She had progressive dyspnea on exertion, accompanied by symptoms of dry cough, muscle weakness, dry mouth, easy bruising and constipation without weight loss for approximately 9 months. During this time, she was also diagnosed with an idiopathic pulmonary embolus with initiation of warfarin.
PMH, SH, FH
During an extensive work-up for these symptoms she was found to have a Ca2+ channel antibody, with concern raised for possible paraneoplastic etiology, as positron emission tomography (PET) imaging also revealed abnormal uptake in lungs along with multiple lymph nodes, pancreatic tail, decreased cerebral metabolism suggestive of a diffuse encephalopathy and bilateral pulmonary infiltrates with cavitation in the lingula. She was also noted to have anemia and thrombocytopenia. Of note, she was up-to-date on all recommended cancer screenings.
Physical Examination
The patient was febrile (39°C), tachypneic (30 breaths/min) and tachycardic (110 beats/min) but blood pressure was normal (110/68 mm Hg). Otherwise physical examination was unremarkable.
Laboratory
CBC: Hemoglobin 9.4 g/dL, white blood cell count 6,200 cells/mcL, platelet count 45,000/mcl
Lactate 1.8 mmol/L
INR: 2.1
Radiography
Admission chest x-ray is shown in figure 1 and the PET scan obtained prior to admission in figure 2.
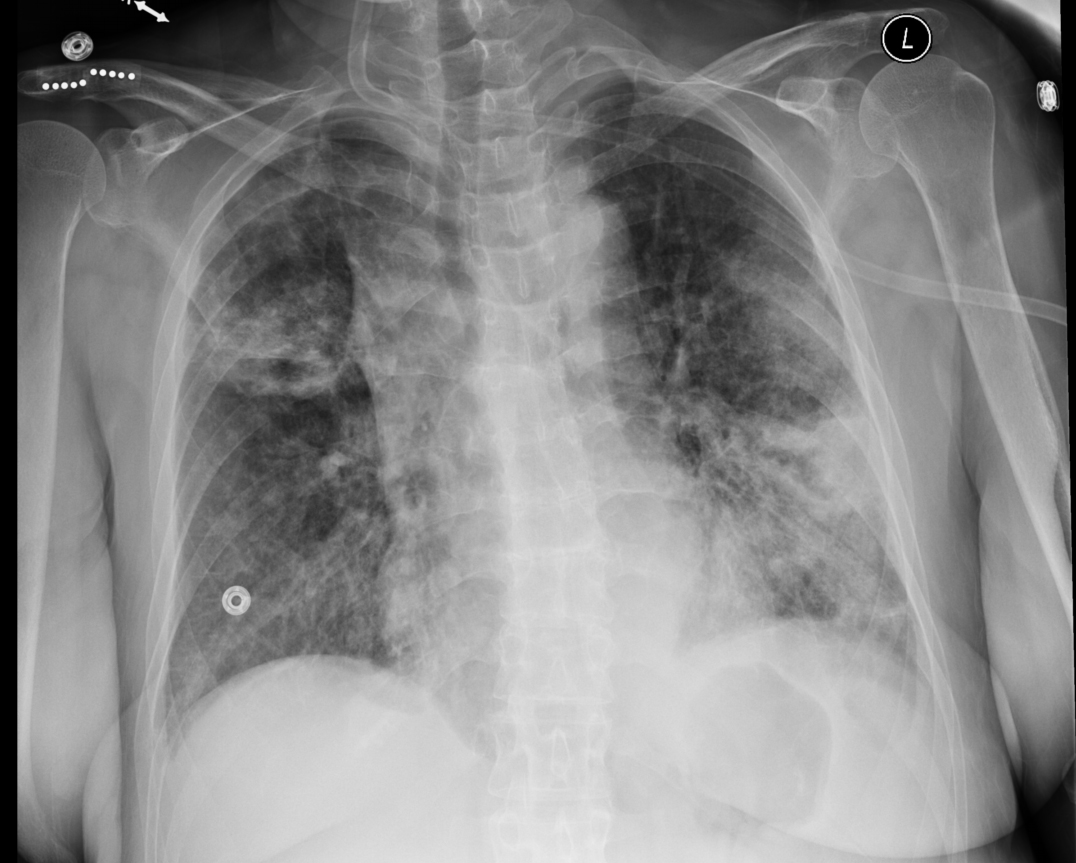
Figure 1. Admission chest x-ray.
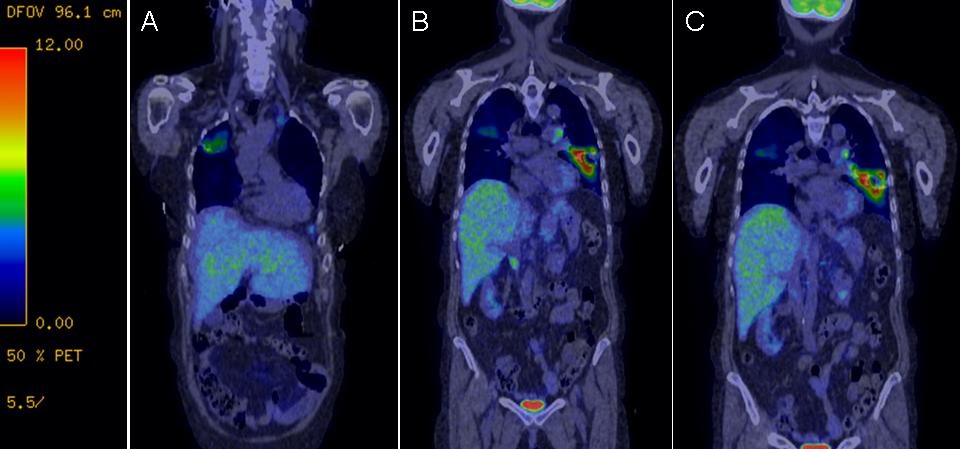
Figure 2. Representative coronal images of the PET scan obtained prior to admission showing abnormal uptake in lungs along with multiple lymph nodes, pancreatic tail, decreased cerebral metabolism suggestive of a diffuse encephalopathy and bilateral pulmonary infiltrates with cavitation in the lingula.
Which of the following should be done on admission?
- Blood culture, sputum culture and urine culture
- Broad spectrum antibiotic coverage
- Intravenous fluids
- Urine culture
- All of the above
Reference as: Cawcutt K, Tosh P, Elmer J, Copeman S, Rivera C. October 2013 pulmonary case of the month: a hidden connection. Southwest J Pulm Crit Care. 2013;7(4): . doi: http://dx.doi.org/10.13175/swjpcc108-13 PDF