Stuart F. Quan, M.D.*†
Daniel Combs, M.D.‡ ¶
Sairam Parthasarathy, M.D.†§ ¶
*Division of Sleep and Circadian Disorders, Brigham and Women’s Hospital, Harvard Medical School, Boston, MA USA
†Asthma and Airways Research Center, University of Arizona College of Medicine, Tucson, AZ USA
‡Department of Pediatrics, University of Arizona College of Medicine, Tucson, AZ USA
§Department of Medicine, University of Arizona College of Medicine, Tucson, AZ USA
¶ Center for Sleep and Circadian Sciences, University of Arizona Health Sciences Center, Tucson, AZ USA
Abstract
Introduction: Weekend oversleep or catchup sleep is a frequent occurrence in children, but there are relatively little data concerning its impact on weight and blood pressure. The aim of this study was to assess the association between sleep duration and oversleep, and weight and blood pressure in adolescents.
Methods: Sleep duration, weight and blood pressure of 327 children (51.4% boys, mean age 13.3 + 1.7 years) who had polysomnograms performed during both exam cycles of the Tucson Children’s Assessment of Sleep Apnea study (TuCASA) were analyzed. Sleep duration on school nights and non-school nights was used to compute a weighted average of child and parent reported overall sleep duration respectively. Oversleep was defined as the difference between self and parent reported weekend sleep and weekday sleep separately. Simple correlations between overall sleep duration, sleep on school and non-school nights and oversleep, and blood pressure, standardized body mass index (BMI), snoring, respiratory disturbance index (RDI) and age were calculated. Significant bivariate associations then were used to develop multivariate partial correlation models.
Results: Unadjusted negative correlations with BMI were noted for parent reported total sleep duration at the 1st exam cycle, parent and child reported total sleep and school night sleep duration, and parent reported non-school night sleep duration at the 2nd exam cycle. Additionally, for BMI, positive correlations were observed for log RDI at both exam cycles and snoring at the 2nd exam cycle. For blood pressure, there were positive associations with age, parent reported oversleep, caffeine consumption and snoring. Additionally, for blood pressure, negative relationships were observed with parent reported total sleep duration at the 1st exam cycle, and parent and child reported total sleep and school night sleep durations at the 2nd exam cycle. Partial correlations found that BMI was negatively correlated with parent reported total sleep duration at the 1st exam cycle and parent reported total sleep duration at the 2nd exam cycle, and positively correlated with snoring and log RDI at both exam cycles. Systolic blood pressure was only associated with age and snoring. Diastolic blood pressure was positively correlated with age and caffeine consumption, and negatively correlated with parent reported total and school night sleep duration. Oversleep and child reported sleep duration were not represented in any of these models.
Conclusion: Lower amounts of sleep especially on school nights is associated with higher body weight and blood pressure. Oversleep was not associated with either body weight or blood pressure.
Introduction
Insufficient sleep in children is associated an increased likelihood of negative behavioral and physical health consequences (1). In particular, short sleep duration has been linked to weight gain and greater risk of obesity, (2-5) and hypertension (6-9). Sleep disordered breathing (SDB) in children also has been implicated as a factor in elevations in blood pressure (10-13). Therefore, it is unclear whether sleep duration and SDB are independent risk factors for this condition.
Weekend oversleep occurs when sleep on weekends exceeds sleep occurring on weekdays. Recently, it was observed in children that greater amounts oversleep were associated with a reduced likelihood of being overweight (4). It was suggested that oversleep represented a compensatory behavior in children for insufficient sleep during weeknights and that it was protective against the deleterious impact of inadequate sleep. Similarly, in adults, oversleep has been associated with a decreased risk of hypertension (14). However, there have been no previous studies of the relationship between oversleep and blood pressure in children.
The Tucson Children’s Assessment of Sleep Apnea Study (TuCASA) was a longitudinal cohort study to assess the impact of SDB on a variety of physiologic and behavioral endpoints (15). The goal of this analysis was to examine whether sleep duration, SDB and oversleep were associated with weight and blood pressure in adolescent children in a general population cohort as represented by TuCASA.
Methods
Subjects and Study Design: Details of the TuCASA study design have been published previously (15, 16). Briefly, 6-11 year-old Hispanic and Caucasian children from the Tucson Unified School District (TUSD) were recruited to undergo unattended home polysomnography. In addition, demographic and anthropometric information was obtained and a neurocognitive assessment performed. From 1999-2004, 503 children aged 6-11 years completed home polysomnograms (Exam Cycle 1). Approximately five years later (Exam Cycle 2, mean 4.7 years), 348 children participated in the second phase of the study; 319 children had home visits where acceptable in-home polysomnography was completed a second time. On both occasions, all of the families completed sleep screening, sleep habits, and morning questionnaires. At the time of the second phase of the study, a comprehensive dietary and physical activity assessment was performed as well (17). The TuCASA study was approved by the University of Arizona Institutional Review Board (IRB) as well as the TUSD Research Committee.
Data collection: The methods for obtaining data have been previously described (11, 15, 16). In brief, for both exam cycles, a two person team arrived at the home approximately one hour before the child’s normal bedtime. Prior to performing any study procedures, parents gave informed consent and the child gave assent to the study using language appropriate forms approved by the IRB. Each child’s height, weight, neck circumference, and blood pressure were measured. One parent was asked to complete a comprehensive Sleep Habits Questionnaire (SHQ) that inquired about their child’s sleep history, sleep characteristics and additional questions regarding parental health including smoking status. For the 2nd exam cycle, the child was asked to complete a SHQ, and a dietary and physical activity questionnaire as well.
Parent and Child Reported Sleep Durations: The SHQ for both parent and child inquired about hours of sleep on school nights and non-school nights. Overall parent and child sleep durations were estimated by computing a weighted average ([school night sleep x 5] + [non-school night sleep x 2] / 7).
Blood Pressure (BP): After a few minutes of rest while seated, the child’s BP was measured in triplicate from the right arm using a portable mercury sphygmomanometer and standardized techniques. The appropriate BP cuff was selected according to the measured arm size (upper arm circumferences of 6-15 cm, infant cuff, 16-22 cm, child cuff, and 23-30 cm, regular-sized adult cuff). The initial cuff inflation pressure was determined by adding 30 mm Hg to the palpated systolic BP. Cuff deflation was at 2 mm/second. At least 30 seconds elapsed between each of the 3 successive measurements. The mean of the final 2 of 3 BP measurements was used for the analyses in this report. Blood pressure percentiles based on height, age and gender were calculated using data from the Centers for Disease Control (CDC) (18).
Obesity: Height was obtained using a folding ruler on a level surface after removal of shoes, and the head in the Frankfort plane. Weight was measured on a platform scale. A standardized BMI z score was calculated using an equation from the CDC which adjusted for age, sex and ethnicity (http://www.cdc.gov/nccdphp/dnpao/growthcharts/resources/sas.htm).
Polysomnography: A single, unattended overnight polysomnogram was obtained using the Compumedics PS-2 system (Abbotsford, Victoria, Australia). The following signals were acquired as part of the TuCASA montage: C3/A2, C4/A1 electroencephalogram (EEG), right and left electrooculogram, a bipolar submental electromyogram, thoracic and abdominal displacement (inductive plethysmography), airflow (nasal/oral thermistor), nasal pressure cannula, finger pulse oximetry, ECG (single bipolar lead), snoring microphone, body position (Hg gauge sensor), and ambient light (sensor attached to the vest to record on/off).
Scoring of the polysomnograms was performed by a single registered polysomnographic technologist using Rechtschaffen and Kales criteria (19). Apneas were scored if the amplitude (peak to trough) of the airflow signal using the thermistor decreased below at least 25% of the amplitude of baseline breathing (identified during a period of regular breathing with stable oxygen levels), if this change lasted for more than 6 seconds or 2 breath cycles. Hypopneas were designated if the amplitude of any respiratory signal decreased below (approximately) 70% of the amplitude of baseline and if the thermistor signal did not meet the criterion for apnea. Central events were marked if no displacement was noted on both the chest and abdominal inductance channels. However, central events that occurred after movement were not included. Otherwise, events were scored as obstructive. After full scoring, analysis software was used to link each event to data from the oxygen saturation and EEG channels. The Respiratory Disturbance Index (RDI) was defined as the number of respiratory events (apneas and hypopneas) per hour of the total sleep time. For this analysis, a 3% oxygen desaturation was required for an event to be counted in the total RDI.
Data: AnalysisDescriptive data are presented as mean + standard deviation (SD) or as percentages. The distributions of RDI and mg caffeine consumption were skewed with some children having values of zero. Therefore, RDI at both exam cycles and caffeine consumption were log transformed. To adjust for zero values, a small number (0.01) was added to each value before the log transformation. Analyses of RDI and caffeine consumption were subsequently performed using log transformed values.
To determine the relationships between the physiologic attributes of weight and blood pressure at the 2nd exam cycle, and variables representing sleep duration, sleep disordered breathing, and caffeine consumption and age, Pearson correlation coefficients were computed. Incorporating only those variables that demonstrated significant bivariate correlations, multivariate models were constructed by calculating partial correlations. Analyses were performed using IBM SPSS Statistics, V24.
Results
There were 327 children (51.4% boys, mean age 13.3+ 1.7 years) who had PSGs performed during both TuCASA exam cycles. In comparison to children who only participated in the 1st exam cycle, there were no differences with respect to age, standardized BMI, RDI, sleep duration on school nights and non-school nights and 1st exam cycle systolic blood pressure (data not shown). However, 1st exam cycle diastolic blood pressure was slightly higher in those who participated in both exam cycles (60.5 + 9.5 vs. 58.4 + 10.3 mmHg, p<0.05).
Analyses of the relationships of household smoking with BMI and blood pressure showed no differences between children living in households with smokers and those with non-smokers. Similarly, there were no associations with physical activity (data not displayed).
Shown in Table 1 are mean values for sleep, anthropometric and blood pressure variables.
Table 1: Mean Values for Sleep, Anthropometric and Blood Pressure Data.*
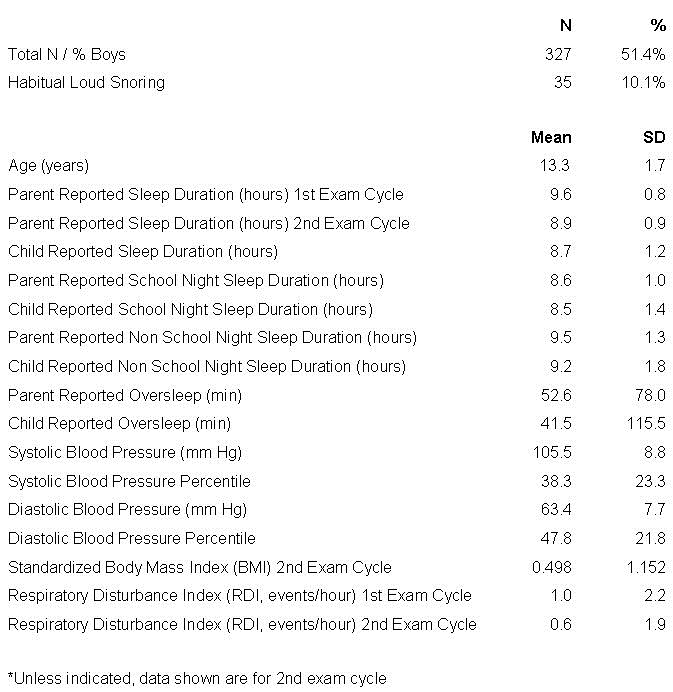
Of note is that parent reported sleep duration declined from the 1st (9.6+0.8 hours) to the 2nd exam cycle (8.9+0.9 hours). Parent reported sleep durations (overall, school night, non-school night and oversleep) were greater than corresponding child reported values.
Unadjusted correlations between standardized BMI and blood pressure, and sleep duration metrics, log RDI, age, caffeine consumption and snoring are provided in Table 2.
Table 2. Unadjusted Correlations with BMI and Blood Pressure.
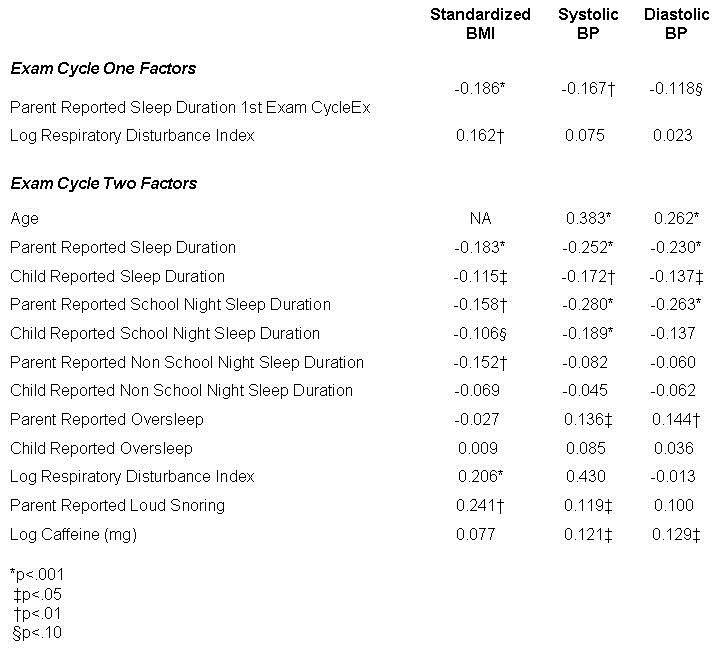
For standardized BMI, significant negative associations with standardized BMI were present for parent reported total sleep duration at the 1st exam cycle, parent and child reported total sleep and school night sleep duration, and parent reported non-school night sleep duration at the 2nd exam cycle. Additionally, for standardized BMI, positive correlations were observed for log RDI at both exam cycles and snoring at the 2nd exam cycle. For blood pressure, there were positive associations with age, caffeine consumption, oversleep and snoring. Additionally, for blood pressure, negative relationships were observed with parent reported total sleep duration at the 1st exam cycle, and parent and child reported total sleep and school night sleep durations at the 2nd exam cycle.
Partial correlations representing multivariate models including only those variables with significant univariate correlations are shown in Table 3.
Table 3. Partial Correlations with BMI and Blood Pressure.
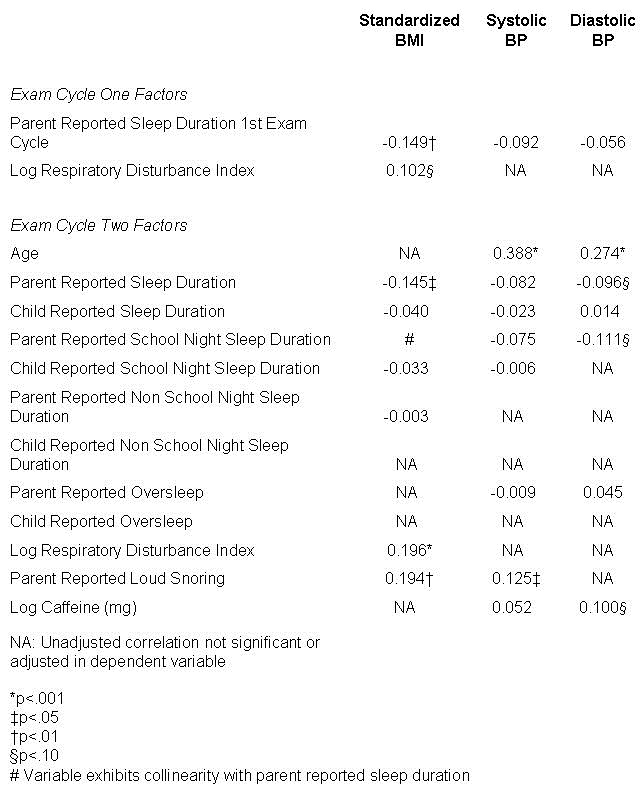
Standardized BMI was negatively correlated with parent reported total sleep duration at the 1st exam cycle, parent reported total sleep duration at the 2nd exam cycle, and positively correlated with snoring and log RDI at both exam cycles. Parent reported school night sleep duration exhibited multicollinearity with other sleep duration metrics. Systolic blood pressure was only associated with age and snoring. Diastolic blood pressure was positively correlated with age and weakly positively correlated with caffeine consumption. It also was weakly negatively correlated with parent reported total and school night sleep duration. Analyses using blood pressure expressed as gender, age and height-adjusted percentiles yielded similar findings (data not shown). Oversleep was not represented in any of these models.
Discussion
The major findings from this analysis were that sleep duration was inversely associated with BMI and to a lesser extent with blood pressure. However, there was no association between oversleep and BMI or blood pressure. Thus, overall sleep duration, but not oversleep, is an important behavioral factor affecting body weight and blood pressure in children.
We observed that parent reported sleep duration overall was inversely correlated with BMI. Our findings are consistent with previous studies that have also found that less sleep in children is associated with greater body weight (2, 3, 5). However, our observation that there was collinearity with parent reported school night sleep duration emphasizes the importance of obtaining adequate sleep during the week. Several mechanisms have been proposed to explain why reduced sleep results in greater body weight. These include alterations in the hormonal processes that regulate carbohydrate metabolism and increase the desire to consume caloric dense foods, and greater available time to eat (20). In a previous analysis of food intake in the TuCASA study, we did not find a relationship between dietary composition and body weight (17). Thus, it is unclear what underlying mechanism explains our finding.
Not surprisingly, age was the primary determinant of blood pressure in our analysis. This is consistent with the normal maturation in children’s blood pressure. However, there was a weak negative correlation between parent reported total and school night sleep durations and diastolic blood pressure. These findings are consistent with previous observations linking reduced sleep duration to higher blood pressure and hypertension in children (7-9). Proposed mechanisms for this relationship include heightened sympathetic nervous system activity and greater exposure to higher daytime blood pressures (6).
A weak association was also noted between diastolic blood pressure and caffeine consumption. In one study in adolescents, a dose response in diastolic but not systolic blood pressure was observed after acute administration of caffeine (21). However, this specificity has not always been found (22). Whether caffeine consumption is a significant risk factor in development of childhood hypertension is unclear. Although a recent large analysis of the NHANES cohort found that the prevalence of elevated blood pressure in children has declined in recent years, a corresponding reduction in caffeine consumption was not statistically significant (23).
In contrast to the inverse associations between parent reported sleep duration and BMI and blood pressure, no relationships were observed between these endpoints and oversleep. Thus, our findings differ from those of Kim et al who found that oversleep exerted a protective effect on weight in children (4). The explanation for this discordance is unclear, but racial and ethnic differences may have been a factor. Our cohort was comprised of Hispanic and Caucasian children and there were systematic differences in bedtime and sleep duration between Hispanics and Caucasian children. Specifically, parent-reported sleep duration during weekdays was shorter in Hispanic than in Caucasian children which appeared to be attributable to a later bedtime in the Hispanic children (24). The children in the afore-mentioned Kim et al study were Korean and the protective effect of oversleep on weight may be attributable to racial, socio-cultural, or dietary differences.
We found that sleep disordered breathing as represented by the RDI and snoring also impacted BMI and blood pressure. This is consistent with our previous findings (11), and others related to SDB and blood pressure in children (10, 12, 13).
In contrast to the associations between parent reported sleep duration and BMI and blood pressure, multivariate analyses failed to confirm any associations between child reported sleep duration and these outcomes. In addition, parent reported sleep times were greater than those reported by their children. Children as young as 8 years can provide meaningful health information when developmentally appropriate instruments are utilized (25). With respect to sleep, the report of the child may be quite different from a parent’s perception (26). Furthermore, both could differ from objective assessment. In the current study, univariate analyses indicated that both child and parent report of sleep duration were associated with BMI and blood pressure. However, only parent report was significant on multivariate analyses. It is possible that greater variability in the child reports was in part responsible for the failure to detect any significant associations. Regardless, it appears that parent reported sleep time represents a better signal than child report for any associations with body weight or blood pressure.
Major limitations to this analysis include a relatively small number of children in comparison to other cohorts and reliance on parent and children reporting of sleep durations. Although polysomnography was performed as part of TuCASA, there was no consistency as to whether they were performed on school or non-school nights. Furthermore, because only a single night of study was recorded, calculation of oversleep would not have been possible. Despite these limitations, TuCASA has several strengths including standardized data collection from a general population cohort and objective documentation of the presence of sleep disordered breathing.
In conclusion, reductions in sleep duration are associated with higher body weight and blood pressure. Reductions in school night sleep are particularly important. However, oversleep does not appear to have an impact on either body weight or blood pressure.
Acknowledgments
This work was supported by grant HL 62373 from the National Heart Lung and Blood Institute.
References
- Paruthi S, Brooks LJ, D'Ambrosio C, et al. Consensus Statement of the American Academy of Sleep Medicine on the Recommended Amount of Sleep for Healthy Children: Methodology and Discussion. J Clin Sleep Med. 2016;12(11):1549-61. [CrossRef] [PubMed]
- Li L, Zhang S, Huang Y, Chen K. Sleep duration and obesity in children: A systematic review and meta-analysis of prospective cohort studies. J Paediatr Child Health. 2017;53(4):378-85. [CrossRef] [PubMed]
- Ruan H, Xun P, Cai W, He K, Tang Q. Habitual Sleep Duration and Risk of Childhood Obesity: Systematic Review and Dose-response Meta-analysis of Prospective Cohort Studies. Sci Rep. 2015;516160. [CrossRef][PubMed]
- Kim CW, Choi MK, Im HJ, et al. Weekend catch-up sleep is associated with decreased risk of being overweight among fifth-grade students with short sleep duration. J Sleep Res. 2012;21(5):546-51. [CrossRef] [PubMed]
- Fatima Y, Doi SA, Mamun AA. Longitudinal impact of sleep on overweight and obesity in children and adolescents: a systematic review and bias-adjusted meta-analysis. Obes Rev. 2015;16(2):137-49. [CrossRef] [PubMed]
- Dean E, Bloom A, Cirillo M, et al. Association between habitual sleep duration and blood pressure and clinical implications: a systematic review. Blood Press. 2012;21(1):45-57. [CrossRef] [PubMed]
- Guo X, Zheng L, Li Y, et al. Association between sleep duration and hypertension among Chinese children and adolescents. Clin Cardiol. 2011;34(12):774-81. [CrossRef] [PubMed]
- Javaheri S, Storfer-Isser A, Rosen CL, Redline S. Sleep quality and elevated blood pressure in adolescents. Circulation. 2008;118(10):1034-40. [CrossRef] [PubMed]
- Kuciene R, Dulskiene V. Associations of short sleep duration with prehypertension and hypertension among Lithuanian children and adolescents: a cross-sectional study. BMC Public Health. 2014;14255-2458-14-255. [CrossRef] [PubMed]
- Bixler EO, Vgontzas AN, Lin HM, et al. Blood pressure associated with sleep-disordered breathing in a population sample of children. Hypertension. 2008;52(5):841-6. [CrossRef] [PubMed]
- Enright PL, Goodwin JL, Sherrill DL, Quan JR, Quan SF, Tucson Children's Assessment of Sleep Apnea study. Blood pressure elevation associated with sleep-related breathing disorder in a community sample of white and Hispanic children: the Tucson Children's Assessment of Sleep Apnea study. Arch Pediatr Adolesc Med. 2003;157(9):901-4. [CrossRef] [PubMed]
- Kwok KL, Ng DK, Chan CH. Cardiovascular changes in children with snoring and obstructive sleep apnoea. Ann Acad Med Singapore. 2008;37(8):715-21. [PubMed]
- Nisbet LC, Yiallourou SR, Walter LM, Horne RS. Blood pressure regulation, autonomic control and sleep disordered breathing in children. Sleep Med Rev. 2014;18(2):179-89. [CrossRef] [PubMed]
- Hwangbo Y, Kim WJ, Chu MK, Yun CH, Yang KI. Association between weekend catch-up sleep duration and hypertension in Korean adults. Sleep Med. 2013;14(6):549-54. [CrossRef] [PubMed]
- Goodwin JL, Enright PL, Kaemingk KL, et al. Feasibility of using unattended polysomnography in children for research--report of the Tucson Children's Assessment of Sleep Apnea study (TuCASA). Sleep. 2001;24(8):937-44. [PubMed]
- Goodwin JL, Kaemingk KL, Mulvaney SA, Morgan WJ, Quan SF. Clinical screening of school children for polysomnography to detect sleep-disordered breathing--the Tucson Children's Assessment of Sleep Apnea study (TuCASA). J Clin Sleep Med. 2005;1(3):247-54. [PubMed]
- Drescher AA, Goodwin JL, Silva GE, Quan SF. Caffeine and screen time in adolescence: associations with short sleep and obesity. J Clin Sleep Med. 2011;7(4):337-42. [CrossRef] [PubMed]
- National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114(2 Suppl 4th Report):555-76. [PubMed]
- Rechtschaffen A, Kales A. A Manual of Standardized Terminology,
Techniques and Scoring System for Sleep Stages of Human Subject. Washington, D.C.: US Government Printing Office, National Institute of Health Publication, 1968. - Ash T, Taveras EM. Associations of short sleep duration with childhood obesity and weight gain: summary of a presentation to the National Academy of Science's Roundtable on Obesity Solutions. Sleep Health. 2017;3(5):389-92. [CrossRef] [PubMed]
- Temple JL, Dewey AM, Briatico LN. Effects of acute caffeine administration on adolescents. Exp Clin Psychopharmacol. 2010;18(6):510-20. [CrossRef] [PubMed]
- Temple JL, Ziegler AM, Graczyk A, Bendlin A, Sion T, Vattana K. Cardiovascular responses to caffeine by gender and pubertal stage. Pediatrics. 2014;134(1):e112-9. [CrossRef] [PubMed]
- Xi B, Zhang T, Zhang M, et al. Trends in Elevated Blood Pressure Among US Children and Adolescents: 1999-2012. Am J Hypertens. 2016;29(2):217-25. [CrossRef] [PubMed]
- Combs D, Goodwin JL, Quan SF, Morgan WJ, Parthasarathy S. Longitudinal differences in sleep duration in Hispanic and Caucasian children. Sleep Med. 2016;1861-6. [CrossRef] [PubMed]
- Riley AW. Evidence that school-age children can self-report on their health. Ambul Pediatr. 2004;4(4 Suppl):371-376. [CrossRef] [PubMed]
- Owens JA, Spirito A, McGuinn M, Nobile C. Sleep habits and sleep disturbance in elementary school-aged children. J Dev Behav Pediatr. 2000;21(1):27-36. [PubMed]
Cite as: Quan SF, Combs D, Parthasarathy S. Impact of sleep duration and weekend oversleep on body weight and blood pressure in adolescents. Southwest J Pulm Crit Care. 2018;16(1):31-41. doi: https://doi.org/10.13175/swjpcc150-17 PDF