Ultrasound for Critical Care Physicians: Sometimes It’s Better to Be Lucky than Smart
 Thursday, June 3, 2021 at 5:00PM
Thursday, June 3, 2021 at 5:00PM Robert A. Raschke MD and Randy Weisman MD
Critical Care Medicine
HonorHealth Scottsdale Osborn Medical Center
Scottsdale, AZ USA
We recently responded to a code arrest alert in the rehabilitation ward of our hospital. The patient was a 47-year-old man who experienced nausea and diaphoresis during physical therapy. Shortly after the therapists helped him sit down in bed, he became unconsciousness and pulseless. The initial code rhythm was a narrow-complex pulseless electrical activity (PEA). He was intubated, received three rounds of epinephrine during approximately 10 minutes of ACLS/CPR before return of spontaneous circulation (ROSC), and was subsequently transferred to the ICU.
Shortly after arriving, a 12-lead EKG was performed (Figure 1), and PEA recurred.
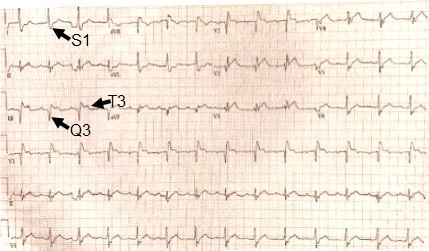
Figure 1. EKG performed just prior to second cardiopulmonary arrest showing S1 Q3 T3 pattern (arrows).
Approximately ten-minutes into this second episode of ACLS, a cardiology consultant informed the code team of an S1,Q3,T3 pattern on the EKG. A point-of-care (POC) echocardiogram performed during rhythm checks was technically-limited, but showed a dilated hypokinetic right ventricle (see video 1).
Video 1. Echocardiogram performed during ACLS rhythm check: Four-chamber view is poor quality, but shows massive RV dilation and systolic dysfunction.
Approximately twenty-minutes into the arrest, 50mg tissue plasminogen activator (tPA) was administered, and return of spontaneous circulation (ROSC) achieved two minutes later. A tPA infusion was started. The patient’s chart was reviewed. He had received care in our ICU previously, but this wasn’t immediately recognized because he had subsequently changed his name of record to the pseudonym “John Doe” (not the real pseduonym), creating two separate and distinct EMR records for the single current hospital stay. Review of the first of these two records, identified by his legal name, revealed he had been admitted to our ICU one month previously for a 5.4 x 3.6 x 2.9 cm left basal ganglia hemorrhage. We stopped the tPA infusion.
On further review of his original EMR is was noted that two weeks after admission for intracranial hemorrhage, (and two weeks prior to cardiopulmonary arrest), he had experienced right leg swelling and an ultrasound demonstrated extensive DVT of the right superficial femoral, saphenous, popliteal and peroneal veins. An IVC filter had been due to anticoagulant contraindication. The patient’s subsequent rehabilitation had been progressing well over the subsequent two weeks and discharge was being discussed on the day cardiopulmonary arrest occurred.
On post-arrest neurological examination, the patient gave a left-sided, thumbs-up to verbal request. Ongoing hypotension was treated with a norepinephrine infusion and inhaled epoprostenol. An emergent head CT was performed and compared to a head CT from four weeks previously (Figure 2), showing normal evolution of the previous intracranial hemorrhage without any new bleeding.
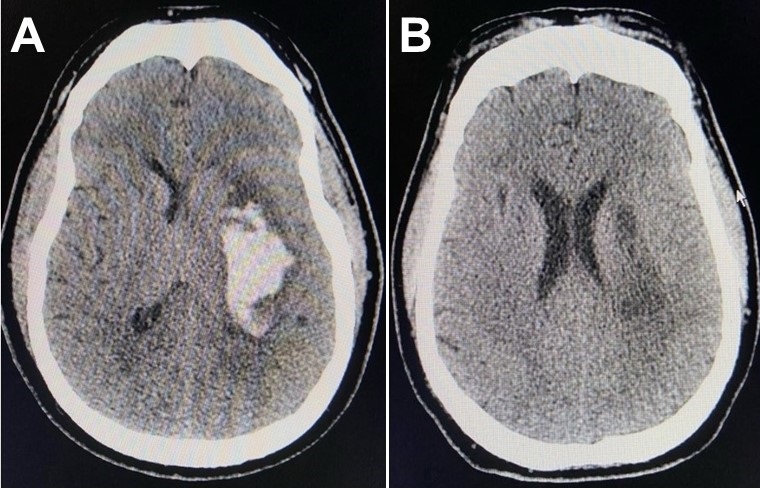
Figure 2. CT brain four weeks prior to (Panel A), and immediately after cardiopulmonary arrest and administration of tPA (Panel B), showing substantial resolution of the previous intracranial hemorrhage.
A therapeutic-dose heparin infusion was started. An official echo confirmed the findings of our POC echo performed during the code, with the additional finding of McConnell’s sign. McConnell’s sign is a distinct echocardiographic finding described in patients with acute pulmonary embolism with regional pattern of right ventricular dysfunction, with akinesia of the mid free wall but normal motion at the apex (1). A CT angiogram showed bilateral pulmonary emboli, and interventional radiology performed bilateral thrombectomies. Hypotension resolved immediately thereafter. The patient was transferred out of the ICU a few days later and resumed his rehabilitation.
A few points of interest:
- IVC filters do not absolutely prevent life-threatening pulmonary embolism (2,3).
- Sometimes, serendipity smiles, as when the cardiologist happened into the room during the code, and provided an essential bit of information.
- Emergent POC ultrasonography is an essential tool in the management of PEA arrest of uncertain etiology.
- Barriers to access of prior medical records can lead to poorly-informed decisions. But in this case, ignorance likely helped us make the right decision.
- Giving lytic therapy one month after an intracranial hemorrhage is not absolutely contra-indicated when in dire need.
- As the late great intensivist, Jay Blum MD used to say: “Sometimes it’s better to be lucky than smart.”
References
- Ogbonnah U, Tawil I, Wray TC, Boivin M. Ultrasound for critical care physicians: Caught in the act. Southwest J Pulm Crit Care. 2018;17(1):36-8. [CrossRef]
-
Urban MK, Jules-Elysee K, MacKenzie CR. Pulmonary embolism after IVC filter. HSS J. 2008 Feb;4(1):74-5. [CrossRef] [PubMed]
-
PREPIC Study Group. Eight-year follow-up of patients with permanent vena cava filters in the prevention of pulmonary embolism: the PREPIC (Prevention du Risque d'Embolie Pulmonaire par Interruption Cave) randomized study. Circulation. 2005 Jul 19;112(3):416-22. doi: [CrossRef] [PubMed]
Cite as: Raschke RA, Weisman R. Ultrasound for Critical Care Physicians: Sometimes It’s Better to Be Lucky than Smart. Southwest J Pulm Crit Care. 2021;22(6):116-8. doi: https://doi.org/10.13175/swjpcc016-21 PDF

Reader Comments