A Failure of Oversight at the VA
 Thursday, September 11, 2014 at 11:29AM
Thursday, September 11, 2014 at 11:29AM On September 8, 2014 the Washington Examiner reported that the Central Office of the VA was allowed to change language in the VA Office of Inspector General (VAOIG) report on delays in patient care at the Phoenix VA Medical Center (1). Crucial language that the VAOIG could not “conclusively” prove that delays in care caused patient deaths at a Phoenix hospital was added to its final report after a draft version was sent to agency administrators for comment. Rep. Jeff Miller, chairman of the House veterans' committee, said "there are significant differences between the final IG report and the draft version ...". The following day Richard Griffin, the acting VAOIG, vigorously defended the independence of his office and bristled at the allegations that the VA was allowed to alter his office's report. However, his denials and indignance seem disingenuous.
To understand why, we need to go back a few years. First, the Phoenix VA overspent its Fee Basis consult budget in 2010. This is the money budgeted to send patients outside the VA for care. To do this a request was filled out and reviewed. Although the Chief of Staff often reviews these requests, this responsibility was delegated to the associate chief of staff for ambulatory care, Keith Piatt. He nearly always approved these requests. Dr. Piatt had other duties including patient care and limited expertise in several of the areas he was requested to evaluate. Furthermore, poor accounting made if unclear if there was sufficient money to pay for these consults. However, rather than questioning why so many patients were outsourced, the VAOIG blamed the problem on the inadequacy of Dr. Piatt's reviews (2). Given this recent IG investigation, it is not surprising that the Phoenix VA administrators were reluctant to outsource patients.
Second, Sam Foote, the initial whistleblower at the Phoenix VA contacted VAOIG in October, 2013. However, according to Foote the VAOIG did not seem to take his allegations seriously, and did what appears to be a superficial investigation (1). So Foote went to the House Committee on Veterans Affairs this past February. Only after the scandal was made public did the VAOIG acknowledge the inadequate care at the Phoenix VA.
Third, the VA prematurely made press releases prior to the release of the VAOIG's final report attempting to exonerate their responsibility (1,3). The final VAOIG report, apparently altered by the VA, was "unable to conclusively assert that the absence of timely quality care caused the deaths of these veterans.” Although this would hardly seem to be an exoneration, media outlets widely reported that whistle-blower allegations were exaggerated and that veterans were not severely affected by wrongdoing at the Phoenix VA medical center. However, in several instances it would seem likely that delayed care contributed to premature patient deaths and would was questioned in a Senate hearing on September 10, 2014 (3).
Fourth, VAOIG investigators corroborated virtually every major allegation of wrongdoing submitted by the first whistle-blower, Dr. Sam Foote (3). Nevertheless, the report and congressional briefing papers contain passages that appear to criticize Foote and his credibility, emphasizing that "the whistle-blower did not provide us with a list of 40 patient names" referring to VA patients Foote said died while awaiting care in Phoenix. This passage was apparently added by VA Central Office. Foote said the portion of the report about him is "false and misleading" because he and other whistle-blowers provided 24 names to inspectors and explained where to identify16 more. The VA report acknowledged that Foote had supplied at least 17 names and that others could not be traced because documentation had been destroyed by VA employees. Rather than defending their indefensible actions, VA Central Office has apparently resorted to denial, indignance, and blaming the whistleblower.
Fifth, the VA continues to obfuscate and obstruct investigations. According to the VAOIG, managers at 13 VA facilities lied to investigators about scheduling problems and other issues and officials at 42 of the 93 sites engaged in manipulation of scheduling, including 19 sites where appointments were cancelled and then rescheduled for the same day to meet on-time performance goals (4). However, it remains unclear whether officials at the Phoenix and Cheyenne VAs have been fired or even suspended. Citing privacy issues, the VA has refused to comment. However, in 2011, Jack Bagdade, a Phoenix VA physician, was fired for violation of the Hatch Act (5). His firing was widely publicized locally. Bagdade was lobbying Senator John McCain for a new research building at the Phoenix VA. Bagdade forwarded an e-mail from McCain's office entitled "Drink Beer for John McCain". If Bagdade's termination for forwarding an e-mail was appropriate punishment (and I am certainly not saying that it was), then what is appropriate punishment for VA administrators who knowingly manipulated patient appointments for their own personal gain, altered records and then lied to investigators?
Several of the VA administrators involved are also licensed physicians and nurses. However, both the Arizona Board of Medical Examiners and Arizona Board of Nursing have been strangely silent. Altering medical records and then lying about it would seem to be a clear violation of the Arizona statues.
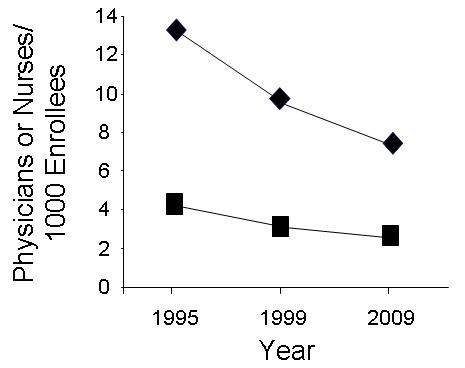
Congress also has to accept some responsibility for their lack of oversight. The problem of inadequate numbers of physicians has been known for years (6). Recently appointed VA Secretary, Robert McDonald, pointed out that the Phoenix VA has now hired 53 additional full-time employees in recent months to help alleviate the appointment backlog (4). He did not mention how many of these employees are physicians nor did he mention how many of the patients were outsourced. However, it seems likely that the hires were merely new administrative personnel to outsource the care of patients. One senior VA official who asked not to be identified said that morale at the VA is poor and doubted that the VA will be able to fill the multiple physician vacancies commenting "Who would want to work here?".
Congress passing a bill to make it easier to fire senior VA administrators suggests they realize there is a problem. However, the legislation still leaves the control of the money up to the very people who misspent it bringing about the present crises. It is also unclear who will do the firing. To date no administrators have been fired despite the law supposedly making this easier. It seems unlikely that any VA administrators are going to fire their colleagues for doing what they are probably also doing or know about. "One of the chief lessons of the VA scandal is that we cannot rely on VA, alone, to effectively identify and correct problems plaguing the department," said Rep. Jeff Miller, chairman of the house veterans' committee. "Oversight and feedback from outside stakeholders is crucial to ensuring VA delivers the benefits and services our veterans have earned." (7). I agree. However, it is doubtful based on their lack of action that either the VAOIG or VA Central Office will take any substantive action to hold those accountable for this scandal and its cover-up. A reasonable solution is to establish a system for local oversight by physicians, nurses and patients (8). Rep. Miller is right, we cannot rely on the VA to fix this problem and oversight is crucial.
Richard A. Robbins, MD*
Editor
References
- Taupin M. IG let veterans affairs officials alter report to absolve agency in phoenix deaths. Washington Examiner. September 8, 2014. Available at: http://washingtonexaminer.com/ig-let-veterans-affairs-officials-alter-report-to-absolve-agency-in-deaths/article/2553035 (accessed 9/10/14).
- VA Office of Inspector General. Review of Alleged Mismanagement of Non-VA Fee Care Funds at the Phoenix VA Health Care System. November 8, 2011. Available at: http://www.va.gov/oig/pubs/VAOIG-11-02280-23.pdf (accessed 9/10/14).
- Wagner D. Critics: VA influenced Inspector General to change Phoenix report for spin-control. Arizona Republic. September 10, 2014. Available at: http://www.azcentral.com/story/news/politics/investigations/2014/09/10/report-phoenix-va-deaths-raises-questions/15375005/ (accessed 9/10/14).
- Daly M. Watchdog: VA managers lied to investigators about delays. Associated Press. September 9, 2014. Available at: http://www.azcentral.com/story/news/nation/politics/2014/09/09/watchdog-va-managers-lied-delays/15334159/ (accessed 9/10/14).
- Kujz S. Valley doctor loses job over invitation to have beer with Arizona senator. ABC News. March 25, 2011. Available at: http://www.abc15.com/news/region-phoenix-metro/central-phoenix/valley-doctor-loses-job-over-invitation-to-have-beer-with-arizona-senator (accessed 9/10/14).
- Robbins RA. VA administrators gaming the system. Southwest J Pulm Crit Care 2012;4:149-54. Available at: http://www.swjpcc.com/editorial/2012/5/5/va-administrators-gaming-the-system.html (accessed 9/10/14).
- Jordan B. Congressman takes va oversight on the road. Military.com news. August 12, 2014. Available at: http://www.military.com/daily-news/2014/08/12/congressman-takes-va-oversight-on-the-road.html (accessed 9/10/14).
- Robbins RA. VA administrators breathe a sigh of relief. Southwest J Pulm Crit Care. 2014;8(6):336-9. [CrossRef]
*The views expressed are those of the author and do not necessarily represent the views of the Arizona, New Mexico, Colorado or California Thoracic Societies or the Mayo Clinic.
Reference as: Robbins RA. A failure of oversight at the VA. Southwest J Pulm Crit Care. 2014;9(3):179-82. doi: http://dx.doi.org/10.13175/swjpcc119-14 PDF