Profiles of Medical Courage: The Courage to Experiment and Barry Marshall
 Monday, July 2, 2012 at 9:49AM
Monday, July 2, 2012 at 9:49AM “The greatest obstacle to knowledge is not ignorance, it is the illusion of knowledge.”-Daniel Boorstein
Previously, four rather obscure physicians and their courageous acts have been described in this series. Barry Marshall is hardly obscure. Along with Robin Warren he won the 2005 Nobel Prize in Medicine for the discovery that H. pylori was the major cause of ulcers. He has been the subject of numerous articles and interviews. However, his story is so compelling and his courage so remarkable, that it bears repeating.
Figure 1. Barry Marshall (left) and Robin Warren (right) toasting their 2005 Nobel Prize.
Barry Marshall was an obscure medicine resident (registrar) in Perth, Australia in the early 1980’s. He had an unremarkable career as a medical student and as a resident (1). He was working 14 hour days, was married with 4 children, and his wife was finishing her degree in psychology.
Against this hectic background, he took a 6 month gastroenterology rotation during the later half of 1981. As part of his training, he was encouraged to perform a clinical research project each year and asked his supervisor, Dr Tom Waters, if there was a gastroenterology project he could work on. Waters showed him a letter from Robin Warren, a pathologist, which listed patients with curved bacteria present on their stomach biopsies and asked for someone to clinically follow-up the patients. This was radical stuff in the day. Stomachs were thought to be sterile because the acid killed any bacteria. Marshall was especially interested because one of the patients was a woman he had seen on the ward, who had severe stomach pain but no diagnosis. In desperation Marshall had referred her to a psychiatrist and commenced antidepressant medication for want of a better treatment. The only abnormal finding was some redness in the stomach and bacteria on the stomach biopsy.
He went to visit Warren in the basement of Royal Perth Hospital where the Pathology Department was located. It was to be the first of many afternoon visits during the next year. Warren used to drink strong black coffee and smoke small cigars. Marshall also occasionally indulged. Together they would discuss their research while smoking cigars in the in Warren’s office in the basement.
At the end of 1981, Marshall’s gastroenterology rotation was finished and his rotations for 1982 had been assigned. In the midst of his time in training, Marshall continued his research by fitting it around his other duties. It was a particularly frustrating time. Marshall was attempting to culture the bacteria, and although masses of bacteria were seen on the silver stain of the gastric biopsies, cultures showed no growth. However, fate intervened. A methicillin-resistant Staphylococcus aureus (MRSA) outbreak occurred on one of the wards at Royal Perth. Patients were being quarantined and surveillance cultures were being performed on all staff that had been anywhere near the affected ward. One of Marshall’s research gastric biopsies taken on the Maundy Thursday before Easter of 1982 was sent to the microbiology lab as usual. However, the lab was overwhelmed with MRSA cultures and the Easter holiday. There was no time to examine Marshall’s cultures on the Saturday before Easter as normally would have been done. The culture plates remained in the incubator, untouched, from Thursday until the following Tuesday. Small transparent colonies were present on the plates and these proved to be a rather pure culture of a Gram negative rod. Why previous cultures showed no growth was explained when Marshall learned the laboratory staff had been processing his research cultures identically to the routine method used for throat-swab cultures. If nothing was seen on the Petri dish after 48 hours, the cultures were discarded. Prior to this, Marshall had no idea that the cultures were only being incubated for 48 hours.
Now that the bacteria had been cultured, Marshall devised a 100 patient observational study of the culture results along with clinical and demographic data. He chose 100 patients simply because in the days before computer spreadsheets this allowed percentages to be easily calculated. He would stay at the hospital each evening to interview inpatients that were due for endoscopy the next morning. In the morning Marshall would arrive early so he could interview the new outpatients as they were being prepared for their endoscopies. Marshall completed his studies in May, 1982 shortly before assuming his next 6 month residency assignment at Port Hedland, a mining town 1,900 km from Perth. In a frenzied weekend while his wife was packing for the trip, Marshall spent Saturday morning at the gastroenterology department photocopying the 100 endoscopy reports.
According to Marshall the time in Port Hedland was an important period. He was able to score the patients’ endoscopies for the presence or absence of ulcers. He had time to do an extensive literature research and discovered that the curved bacteria described by Warren had been described many times before but ignored. Furthermore, he could find no evidence for the existence of stress in causing ulcers. He also had time to digest the results of his study and prepare it for presentation.
In October, 1982, Marshall presented his findings to the local College of Physicians meeting, where it received a mixed response (Figure 2) (1).
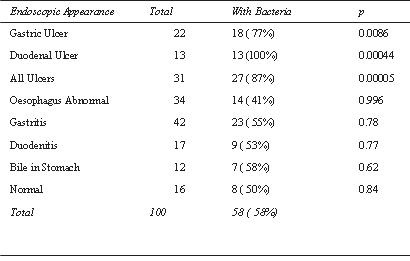
Figure 2. Percentage of patients with bacteria identified on gastric biopsy and their endoscopic appearance.
Marshall’s unrestrained enthusiasm, combined with his youthful appearance and informal manner, apparently fed the skepticism of his audience. Marshall's critics contended that the presence of bacteria in the stomachs of patients with gastric diseases was coincidental, and that the bacteria were probably harmless. Furthermore, the bacteria were seen in the stomach and probably could not explain duodenal ulcers. Lastly, it seemed pretty unlikely that a medicine resident was making a significant observation when previously no one thought the bacteria were important.
At about the same time, Marshall found that his contract at Royal Perth would not be renewed for the following year. Previously unfocused, he now wanted to work in gastroenterology or microbiology and continue his research. However, jobs at Royal Perth were not available. Fate intervened for a second time when Marshall was approached by Drs. Norm Marinovich and Ian Hislop at Fremantle Hospital in Perth who offered Marshall a senior registrar position and continued funding of his research. Fremantle was the third and smallest of the teaching hospitals in Perth but had a tradition of openness and experimentation. In the next two years at Fremantle Marshall had an enthusiastic group of collaborators including Ian Hislop, Norm Marinovich, Harvey Turner, David McGechie, Ross Glancy, Neil Noakes, Graeme Francis, Peter Rogers, Neil Stingemore, and importantly, Peter Smith, the chief (superintendent) of medicine.
While at Fremantle, Marshall was able to confirm that the stomach bacteria observed at Royal Perth Hospital also occurred at Fremantle. Furthermore, nearly all peptic ulcer patients had the organism. Freemantle Hospital was supporting Marshall’s work and there Marshall devised the first effective treatment for peptic ulcer disease consisting of antibiotics and bismuth. However, acceptance of the association of the bacteria with peptic ulcer disease was slow. Practitioners of gastroenterology and the pharmaceutical industry were both heavily invested in the theory that peptic ulcers were caused by emotional stress and stomach acids, and could only be treated with repeated courses of antacid medication. While the reduction of stomach acid often alleviated the existing ulcer, inflammation of the stomach lining usually persisted, and most patients found themselves returning in a year or two with another ulcer. Patients were routinely advised to seek psychiatric counseling, find less demanding employment or make other drastic lifestyle changes to address the purported cause of their disease. Volumes were published detailing the alleged psychological causes of gastric ailments, and ulcers remained a frequently cited example of psychosomatic illness.
In 1983 the Gastroenterological Society of Australia meeting was in Perth. This was great news to Marshall because it provided an opportunity to present his research with little cost. He was so poor he could not afford an airfare to any scientific meetings. He submitted an abstract to the meeting, but to his shock, it was rejected (Figure 3).

Figure 3. Rejection letter of Marshall’s abstract from the Gastroenterogical Society of Australia meeting held in Perth, 2003.
Sixty-seven abstracts had been submitted and 56 were accepted. The Society suggested that Marshall should seek critical review from his colleagues.
The rejection may have been fortunate because in prompted David McGechie from Fremantle to put Marshall in contact Dr Martin Skirrow in the UK. Skirrow arranged for Marshall to present at the European Campylobacter Meeting in September, 1983. There Marshall’s abstract meant with some acceptance and more publicity. In addition to his presentation, Marshall visited Martin Skirrow in Worcester, England, and attended an endoscopy session at the Worcester Infirmary. Martin's registrar, Cliodna McNulty, was able to successfully isolate the stomach bacteria 3 days later, showing that the spiral organism was not merely an Australian phenomenon but was present in ulcer patients in the UK as well.
After the pilot study was completed, Marshall and Warren submitted their work to the medical journal, The Lancet. Editors were initially reluctant to publish their work because they could find no reviewers who believed their results. Skirrow, contacted The Lancet confirming Warren and Marshal’s findings and, in June 1984, they succeeded in publishing their paper (3).
Despite some success, the time at Fremantle was also frustrating. Marshall’s attempts at making an animal model of peptic ulcer disease were unsuccessful. Furthermore, his research was not receiving the type of attention he had hoped. Criticism had become personal. One prominent gastroenterologist dismissed him as "a crazy guy saying crazy things” (4). His wife overheard comments that were disheartening.
Marshall became convinced that in order to have anyone believe an infectious cause he would have to fulfill Koch’s postulates. However, with the absence of an animal model complicating progress, Marshall decided that he could use himself as a model. Fortunately, he was secretive about the experiment. It is unlikely that any human experimentation committee would have approved. Since he probably would have proceeded anyway, Marshall would likely have been fired. Marshall thought that if he was successful he would develop an ulcer or stomach problems from the bacteria probably in a couple of years. Without explanation he asked Ian Hislop to do a baseline endoscopy and a gastric biopsy. As Hislop put the scope down he said, “Barry, I’m not going to ask why I’m doing this.” (5). From around the gastroscope, Marshall gritted out, “Just take the biopsy.” (5). The endoscopy was normal and the biopsy did not show bacteria.
Then Marshall drank bacteria that were cultured from a patient who did not actually have ulcers, just indigestion and gastritis. Furthermore, Marshall was able to eradicate the patient’s infection with antibiotics, so he already knew that he could, if necessary, take a treatment that worked. Instead of being perfectly well and having a silent infection, he started vomiting after about five days. It was a clear liquid, and there was no acid in it. His wife noticed he was ill and questioned him about it. He told her the truth and she was horrified that he infected himself and took the chance of spreading the infection to her and their kids. She demanded he take an antibiotic. He took the antibiotics and was cured but not before getting another endoscopy and biopsy. He had gastritis and bacteria were everywhere. He had fulfilled Koch’s postulates for gastritis, though not for ulcers. Marshall’s self-experimentation was later immortalized by the comic Ulcer Tales which was distributed to many US physicians (Figure 4) (6).

Figure 4. Ulcer Tales, a comic depicting Marshall’s ingestion of Helicobacter.
Even though he was not officially collaborating with Dr. Warren while he was working at Fremantle Hospital in 1983–84, Marshall and Warren met to discuss the papers they were writing for the Lancet and would meet for dinner with their wives. At one of these dinners Marshall described his self-experimentation. Early the next morning Warren had a call from a journalist in the USA at 5 AM. When asked the usual question about "How do you know it's a pathogen and not a harmless commensal?" Warren blabbed the results of Marshall’s self-experimentation. What Warren did not know was that the journalist was from the "Star" newspaper, the grocery store tabloid. This was right up their alley. In the next issue the story appeared, "Guinea-pig doctor discovers new cure for ulcers ... and the cause” (7).
This became one of those serendipitous, life changing events in Marshall’s life. After the Star article appeared, Marshall was continuously contacted by patients in the USA who read the story and were desperate for treatment. Marshall was able to help. He was treating patients by proxy in the USA as early as 1984. The publicity caught the eye of Mike Manhart, a microbiologist working for Proctor and Gamble in the USA. He tracked down Marshall’s publications and realized the economic potential for P & G who made a bismuth drug. It led to Marshall to leave Perth and spending the next ten years spent at University of Virginia.
The tide of acceptance began to turn in the early 1990s. By then Marshall could attend a meeting and receive as much praise as criticism. In February 1994 the NIH held a consensus meeting in Washington DC which ended after 2 days with the statement that the key to treatment of duodenal and gastric ulcer was detection and eradication of Helicobacter pylori (8).
However after 10 years in the US, Marshall and his wife decided it was time to go home. Marshall was awarded the McFarlane Burnet Fellowship which funded his lab at the University of Western Australia allowing him to return to Perth. His worked culminated with Robin Warren and him receiving the Nobel prize in 2005. In typical fashion, Marshall acknowledges those who failed to recognize H. pylori in his autobiography (1). Without them Marshall would have had a very different career. He also notes that one of the truly great things about winning the Nobel Prize in 2005 was that he got to share it and celebrate with those who had been involved in the initial work at Royal Perth and Fremantle Hospital. The Australians might refer to this as “partying with your mates”.
There were many occasions when Marshall was lucky: his meeting with Robin Warren, the MRSA outbreak leading to the first culture of the bacteria, the rejection of his abstract in 1983 and chance meetings with many people who helped and collaborated with him. We should remember Marshall not as much for his good fortune or his brashness in self-experimentation, but in his persistence in challenging the dogma that stomachs are sterile and ulcers result from stress. Marshall continues to lecture and because of his fame some of these lectures are available as videos on the internet. He opened his Nobel prize lecture with the quote from Boorstein that began this article, “The greatest obstacle to knowledge is not ignorance, it is the illusion of knowledge.”(7). It fits Marshall’s story well.
Richard A. Robbins, MD
Editor, Southwest Journal of Pulmonary and
Critical Care
References
- Marshall BJ. Autobiography. Available at Nobelprize.org http://www.nobelprize.org/nobel_prizes/medicine/laureates/2005/marshall-autobio.html (accessed 6/5/2012).
- Marshall BJ. Lecture by Barry Marshall. http://www.nobelprize.org/mediaplayer/index.php?id=1721
- Unidentified curved bacilli in the stomach of patients with gastritis and peptic ulceration. Marshall BJ, Warren JR. Lancet 1984;1(8390):1311-5.
- Barry Marshall Biography. http://www.achievement.org/autodoc/page/mar1bio-1 (accessed 6/5/2012).
- Barry Marshall gastroenterologist. http://www.science.org.au/scientists/interviews/m/marshall.html#Childhoodleanings (accessed 6/5/2012).
- http://www.melanievillines.com/samples/HPComic.pdf (accessed 6/5/2012).
- Marshall BJ. Nobel Prize Lecture. http://www.docstoc.com/docs/77029428/Barry-Marshall-Nobel-Lecture (accessed 6/5/2012).
- http://consensus.nih.gov/1994/1994HelicobacterPyloriUlcer094html.htm (accessed 6/5/2012).
Reference as: Robbins RA. Profiles of medical courage: the courage to experiment and Barry Marshall. Southwest J Pulm Crit Care 2012;5:12-19. (click here for a PDF version of the manuscript)

