Medical Image of the Month: Hepatic Abscess Secondary to Diverticulitis Resulting in Sepsis
 Friday, July 2, 2021 at 8:00AM
Friday, July 2, 2021 at 8:00AM 
Figure 1. An axial, post-contrast CT of the abdomen and pelvis demonstrates an ill-defined, multiloculated, hypodense lesion in the right hepatic lobe most consistent with a hepatic abscess (red circle).
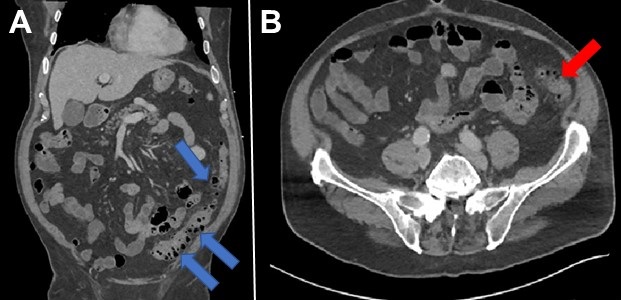 Figure 2. Coronal and axial reconstructions of the post-contrast CT of the abdomen and pelvis demonstrate extensive diverticulosis of the descending and sigmoid colon (blue arrows) with a focal area of fat-stranding in the descending colon consistent with diverticulitis (red arrow) – likely the source of the patient’s hepatic abscess.
Figure 2. Coronal and axial reconstructions of the post-contrast CT of the abdomen and pelvis demonstrate extensive diverticulosis of the descending and sigmoid colon (blue arrows) with a focal area of fat-stranding in the descending colon consistent with diverticulitis (red arrow) – likely the source of the patient’s hepatic abscess.
Clinical Scenario: A 73-year-old man with a previous history of hypertension presented to the hospital with a 4-day history of malaise, myalgias, syncope, nausea, and vomiting. He denied having any fevers, chills, diarrhea, abdominal pain, or recent travel. Upon arrival to the hospital, he was found to be febrile to 103.4°F, and hypotensive with systolic blood pressures in the 80’s. His baseline documented systolic blood pressures from numerous outpatient clinics were in the 110’s. In addition, he was hypoxemic requiring 6 L/min of supplemental oxygen to maintain an adequate oxygen saturation. Physical examination was significant for alteration of his mental status. He denied any abdominal pain with palpation, and there was no rebound tenderness or guarding. His lab work was significant for a leukopenia and thrombocytopenia - new from his previous lab work in our system. A CT of the abdomen and pelvis with contrast demonstrated a multiloculated abscess in the right hepatic lobe (Figure 1). He also had extensive diverticular disease of the descending and sigmoid colon with a focal area of diverticulitis in the descending colon (Figure 2). A CT-guided, percutaneous drain was placed in the right hepatic lobe abscess which grew Streptococcus anginosus and Bacteroides fragilis. With the combination of antibiotics and drainage of the abscess, his clinical condition markedly improved. He was discharged approximately 1 week after admission at his normal baseline.
Discussion: Liver abscess is the most common type of visceral abscess (1). Clinical manifestations include a broad spectrum of symptoms, but the most common are fever (70%–90% of patients) and abdominal pain, usually in the right upper quadrant (50%–75%) (2-4). Liver abscesses can occur because of multiple etiologies to include ascending cholangitis, hematogenous spread from the gastrointestinal tract via portal venous drainage of infectious entities such as diverticulitis and appendicitis, and from hematogenous spread via the hepatic artery. Other etiologies for the development of hepatic abscesses include penetrating trauma or after an invasive procedure (for example biliary instrumentation, transcatheter arterial chemoembolization, percutaneous liver biopsy, or abdominal surgery) (5).
Many bacteria have been described in the pathogenesis of pyogenic abscesses, reflecting the variability among patients and geographic areas. Many aspirated fluid cultures are positive, whereas blood cultures are positive in only 50% of cases (4). Most pyogenic liver abscesses are polymicrobial (4). Traditionally, Escherichia coli has been reported as the most common isolated microbe; however, recent data show that Klebsiella pneumoniae is the most common pathogen in pyogenic liver abscesses (3,4,6).
Management of pyogenic liver abscesses includes imaging-guided drainage and antibiotic therapy. There is considerable variation in clinical practice regarding total antibiotic duration (7). It is recommended that antibiotic therapy be continued for at least 4–6 weeks, but the optimal duration is still unclear (7). Although drainage of single abscesses with a diameter of 5 cm or less can be achieved in some cases, it may not improve outcomes compared with antibiotic treatment alone. In isolated abscesses with a diameter greater than 5 cm, catheter drainage should be considered and is preferred over needle aspiration, although some favor surgical intervention (8). Prompt diagnosis and imaging-guided drainage have been reported to reduce mortality from 65% to 2%–12% (2-4).
Reubender Randhawa MD1, Alan Nyquist MD2, and Tammer El-Aini MD2
1Banner University Medical Center – South Campus, Department of Internal Medicine, Tucson, AZ USA
2Banner University Medical Center – Tucson Campus, Department of Pulmonary and Critical Care
References
- Altemeier WA, Culbertson WR, Fullen WD, Shook CD. Intra-abdominal abscesses. Am J Surg. 1973 Jan;125(1):70-9. [CrossRef] [PubMed]
- Mohsen AH, Green ST, Read RC, McKendrick MW. Liver abscess in adults: ten years experience in a UK centre. QJM. 2002 Dec;95(12):797-802. [CrossRef] [PubMed]
- Rahimian J, Wilson T, Oram V, Holzman RS. Pyogenic liver abscess: recent trends in etiology and mortality. Clin Infect Dis. 2004 Dec 1;39(11):1654-9. [CrossRef] [PubMed]
- Huang CJ, Pitt HA, Lipsett PA, Osterman FA Jr, Lillemoe KD, Cameron JL, Zuidema GD. Pyogenic hepatic abscess. Changing trends over 42 years. Ann Surg. 1996 May;223(5):600-7; discussion 607-9. [CrossRef] [PubMed]
- Wisplinghoff H, Appleton DL. Bacterial infections of the liver. In: Weber O, Protzer U, eds. Comparative hepatitis. Basel, Switzerland: Birkhäuser, 2008; 143–160. [CrossRef]
- Liu Y, Wang JY, Jiang W. An Increasing Prominent Disease of Klebsiella pneumoniae Liver Abscess: Etiology, Diagnosis, and Treatment. Gastroenterol Res Pract. 2013;2013:258514. [CrossRef] [PubMed]
- Molton J, Phillips R, Gandhi M, Yoong J, Lye D, Tan TT, Fisher D, Archuleta S. Oral versus intravenous antibiotics for patients with Klebsiella pneumoniae liver abscess: study protocol for a randomized controlled trial. Trials. 2013 Oct 31;14:364. [CrossRef] [PubMed]
- Zerem E, Hadzic A. Sonographically guided percutaneous catheter drainage versus needle aspiration in the management of pyogenic liver abscess. AJR Am J Roentgenol. 2007 Sep;189(3):W138-42. [CrossRef] [PubMed]
Cite as: Randhawa R, Nyquist A, El-Aini T. Medical image of the month: hepatic abscess secondary to diverticulitis resulting in sepsis. Southwest J Pulm Crit Care. 2021;23(1):5-7. doi: https://doi.org/10.13175/swjpcc019-21 PDF

Reader Comments