Migratory Breast Implant: A Case Report and Brief Review
 Wednesday, July 15, 2020 at 8:00AM
Wednesday, July 15, 2020 at 8:00AM Bush Benjamin MD
Nishal Brahmbhatt MD
Jose F. Santacruz MD
Ramchandani Mahesh MD
Houston Methodist Hospital
Houston, Texas USA
Abstract
A 75-year-old woman with a history of myasthenia gravis status post thymectomy and bilateral breast implants presented with complaints of acute onset shortness of breath and chest pain. Her thymectomy was performed via video-assisted thorascopic surgery (VATS) four months prior to presentation. A CT scan of the chest revealed migration of the left breast implant into the pleural space. She underwent an emergent thoracotomy with removal of the implant and subsequent complete resolution of her symptoms.
Introduction
We present a case of breast implant migration into the pleural space four months after video- assisted thoracoscopic surgery (VATS). A literature review highlights six other known cases of breast implant displacement following VATS. Breast augmentation is the number one cosmetic surgical procedure performed in the United States with the overall number of procedures rising from 2017 to 2018 (1). There are several complications that are associated with this surgical procedure. We present a rare case of breast implant migration into the pleural space after VATS. As the prevalence of breast implantation increases within the general population, thoracic surgeons and pulmonologists need to be aware of the risks of implant migration. Though rare, breast implant migration into the pleural space presents an important post-operative complication that will be explored in this case.
Case Summary
A 75-year-old woman presented to the emergency room with complaints of shortness of breath and left-sided chest pain. Her medical history was significant for chronic bronchiectasis on home oxygen, myasthenia gravis with intermittent exacerbations requiring IVIG and plasma exchange, and bilateral breast implants placed approximately 45 years earlier. Her myasthenia gravis was thought to be associated with a thymoma that was treated with thirty rounds of external beam radiation followed by a VATS thymectomy 4 months prior to presentation. Her thymectomy was well-tolerated with no immediate peri-operative complications. Two weeks post-thymectomy, she was hospitalized with complaints of shortness of breath. A CT scan of the chest revealed subacute appearing fractures of the anterior left 2nd-5th ribs, with interval widening of the anterior 4th left rib interspace and increasing approximation of the left breast prosthesis to the left pleura which was believed to be secondary to her recent thymectomy (Figure 1).

Figure 1. Axial contrast-enhanced CT of the chest shows approximation of the left breast prosthesis to the pleura.
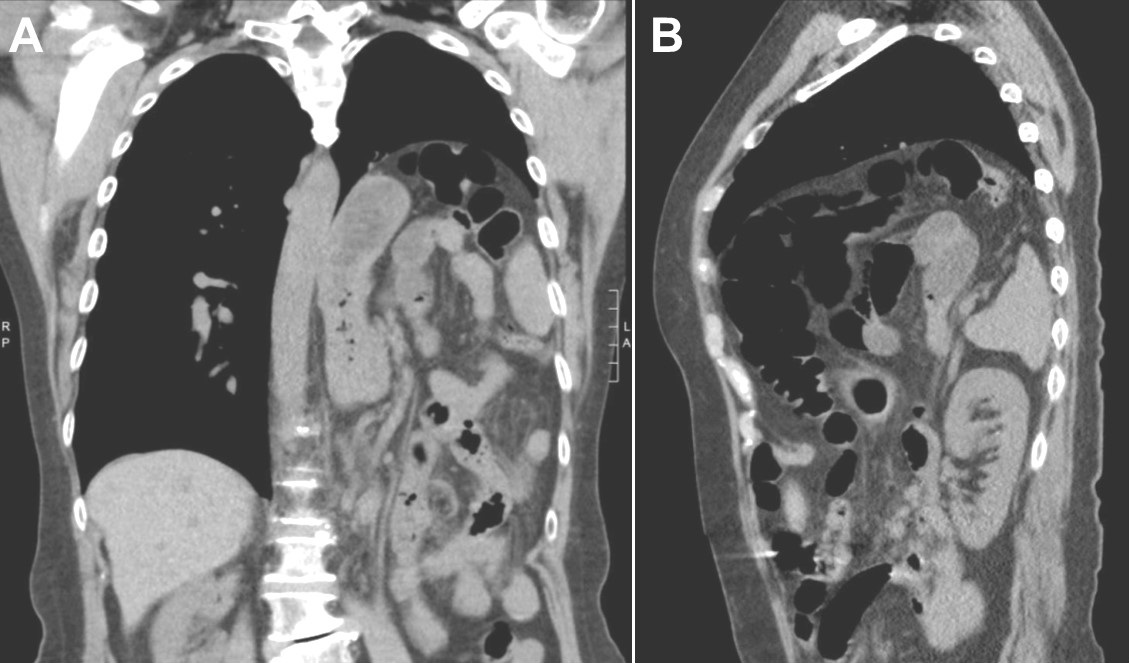
These findings were not thought to be clinically significant and her symptoms were attributed to an exacerbation of her myasthenia gravis. Her symptoms resolved after treatment of an exacerbation of her myasthenia gravis. Two months later, she presented with acute onset of shortness of breath and left-sided chest pain which was new compared to prior symptoms. She also noted that her left breast implanted had moved. Subsequent physical exams noted no identifiable prosthesis along left anterior chest wall which prompted further evaluation. A CTA chest was obtained in the ED which identified interval migration of left breast implant into the posterior left chest (Figure 2).

Figure 2. A: Coronal contrast-enhanced CT of the chest in lung windows performed two months later demonstrates migration of the breast prosthesis into the left pleural space with mass effect resulting in near complete collapse of the left lower lobe. B: Axial contrast-enhanced CT of the chest again demonstrates migration of the left breast prothesis into the left pleural space resulting in near complete collapse of the left lower lobe.
She was emergently taken to operating room for removal of the foreign body from pleural cavity. Prior to operation, the patient expressed her wish to forego further cosmetic operations and desired to simply have her implants removed. After repeat thoracotomy, the expulsed implant was removed. No post-operative complications were noted, symptoms resolved, and she was discharged home on post-op day 3 with continued outpatient monitoring.
Discussion
This case highlights a rare but potentially life-threatening complication of VATS procedures in the setting of a relatively common cosmetic procedure. Given the patient’s history of bronchiectasis and multiple hospitalizations for shortness of breath associated with her myasthenia gravis, her presentation could have initially been misidentified as a recurrent myasthenia gravis exacerbation. The astute observation by the patient of her implant migration is what prompted her physicians to further evaluate the etiology of her symptoms with imaging studies. Additionally, she underwent a VATS procedure for her thymectomy - a procedure generally performed to reduce the risk of complications, minimize recovery time, and for patients who may not tolerate open procedures. However, it should be documented that displacement of breast implants into the pleural space is a potentially severe, albeit rare, complication of VATS.
While pleural damage and potential expulsion of the breast prosthesis is a well-documented complication of breast augmentation, only a handful of cases of breast implant migration associated with VATS procedures have been reported. One case reported by Bruintjes et al. (2) details implant migration in the immediate post-operative period. Another case presented by Sykes et al. (3) reports intrathoracic migration of a breast implant approximately 5 months after a VATS procedure - a timeline similar to our case. Both cases noted small thoracic wall defects upon inspection, which in combination with the negative pressure of the pleural cavity, could account for migration of the breast implant into the pleural space. In our case, the CT surgeon noted a 15 cm left-sided thoracic wall defect communicating with the breast implant capsule during implant retrieval.
Migration of breast implants into the pleural space can cause lung collapse due to mass effect, promote the development of pleural effusions, cause localized inflammatory responses, and increase the risk of infections. Additionally, silicone breast implants have been noted to rupture and seed the pleural space - causing silicosis and scleroderma-like syndromes in women (4,5)
Additionally, the operative note revealed extensive fibrosis and scarring of mediastinal and anterior thoracic wall tissue consistent with her history of radiation therapy. The fibrotic tissue may have contributed to the patient’s presentation by causing delayed healing and a persistent defect in the thoracic wall which allowed for the displacement of the prosthesis. In this case, our patient had previous imaging that showed approximation of the left breast prosthesis to the pleura almost 2 months prior to this significant event. Intervention at that time or closer monitoring with repeat imaging could have potentially adverted this life-threatening event.
As minimally invasive procedures such as VATS are used more commonly and as the prevalence of breast augmentation increases, it is important to highlight the potential life-threatening complications that can arise in such patients. Physicians should consider such complications as to prevent delays in diagnosis and treatment.
References
- ASPS National Clearing House of Plastic Surgery. Plastic Surgery Statistics Report 2018. Available at: https://www.plasticsurgery.org/documents/News/Statistics/2018/plastic-surgery-statistics-report-2018.pdf (accessed 7/13/20).
- Bruintjes MH, Schouten C, Fabré J, van den Wildenberg FJ, Wijnberg DS. Where the PIP is the implant?. J Plast Reconstr Aesthet Surg. 2014;67(8):1148-1150. [CrossRef] [PubMed]
- Sykes JB, Rosella PA. Intrathoracic migration of a silicone breast implant 5 months after video-assisted thoracoscopic surgery. J Comput Assist Tomogr. 2012;36(3):306-307. [CrossRef] [PubMed]
- Gleeson JP, Redmond HP, O'Reilly S. Siliconosis and the long-term implications of silent breast implant rupture. Breast J. 2019;25(5):1002-1003. [CrossRef] [PubMed]
- Wroński J, Bonek K, Stanisławska-Biernat E. Scleroderma-like syndrome in a woman with silicone breast implants - case report and critical review of the literature. Reumatologia. 2019;57(1):55-58. [CrossRef] [PubMed]
Cite as: Benjamin B, Brahmbhatt N, Santacruz SF, Mahesh R. Migratory breast implant: a case report and brief review. Southwest J Pulm Crit Care. 2020;21(1):11-14. doi: https://doi.org/10.13175/swjpcc039-20 PDF