February 2020 Imaging Case of the Month: An Emerging Cause for Infiltrative Lung Abnormalities
 Saturday, February 1, 2020 at 8:00AM
Saturday, February 1, 2020 at 8:00AM Prasad M. Panse MD*, Fiona F. Feller MD†, Yasmeen M. Butt MD‡, Michael B. Gotway MD*
Departments of *Radiology, †Medicine, and ‡Laboratory Medicine
Mayo Clinic, Arizona
Phoenix, Arizona
Clinical History: A 25-year-old man with no previous medical history presented to the Emergency Room with complaints of worsening non-productive cough and fever to 102°F over the previous 7 days. The patient also complained of some nausea, vomiting, and generalized muscle aches. The patient denies rhinorrhea, sore throat, congestion, and diarrhea. The patient also illicit drug use, and drinks alcohol only occasionally. He said he previously smoked 1-2 packs-per day, having quit 6 months earlier.
The patient’s physical examination showed normal vital signs, although his respiration rate was approximately 18/minute. The physical examination showed some mild basilar crackles bilaterally, but was otherwise entirely within normal limits.
Basic laboratory data showed a white blood cell count near the upper of normal= 10.3 x 109 / L (normal, 4–10.8 x 109/L) with a normal platelet count and no evidence of anemia, normal serum chemistries and renal function parameters, and normal liver function tests. The patient was referred for chest radiography (Figure 1).
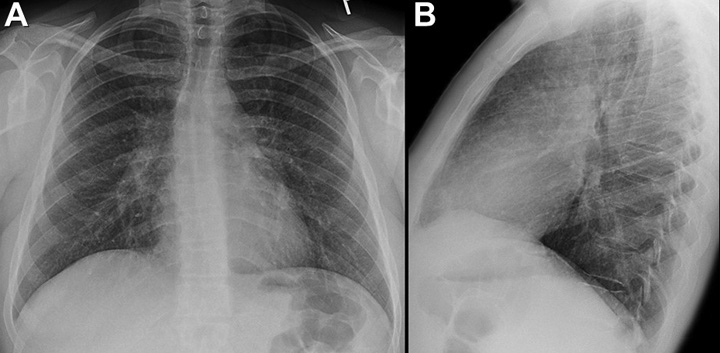
Figure 1. Frontal (A) and lateral (B) chest radiography at presentation.
Which of the following statements regarding the chest radiograph is most accurate? (Click on the correct answer to be directed to the second of fourteen pages)
- The chest radiograph shows bilateral consolidation
- The chest radiograph shows findings suggesting increased pressure pulmonary edema
- The chest radiograph shows mediastinal and peribronchial lymph node enlargement
- The chest radiograph shows mild perihilar infiltration
- The chest radiograph shows normal findings
Cite as: Panse PM, Feller FF, Butt YM, Gotway MB. February 2020 imaging case of the month: an emerging cause for infiltrative lung abnormalities. Southwest J Pulm Crit Care. 2020;20(2):43-58. doi: https://doi.org/10.13175/swjpcc004-20 PDF

