Medical Image of the Month: Mucinous Adenocarcinoma of the Lung Mimicking Pneumonia
 Saturday, January 2, 2021 at 8:00AM
Saturday, January 2, 2021 at 8:00AM 
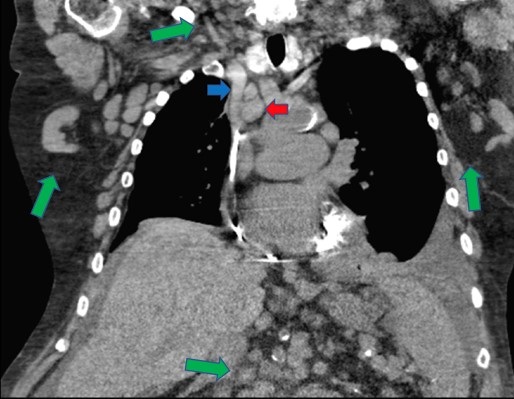
Figure 1. A contrasted, coronal-reformatted CT image of the chest demonstrates unilateral ground glass opacification of the right lung with superimposed interlobular septal thickening (blue arrows). There is also volume loss of the left lung with elevation of the left hemidiaphragm (red arrow).
Clinical Scenario: A 60-year-old man with a history of chronic obstructive pulmonary disease presented to the hospital with worsening shortness of breath over a period of 3 days. He had a 50-pack-year history of smoking, coronary artery disease, and a previous history of a left lung mass of unknown pathology status post left upper lobectomy. He was bought to the emergency room via ambulance after being found at home with oxygen saturations in the 60s. Upon arrival to the emergency room, he required continuous oxygen at 15 L/min to maintain his oxygen saturations above 88%. He had a progressive, markedly productive cough over the last few weeks prior to presentation. He had been treated for pneumonia with multiple courses of antibiotics over the last two months without any significant improvement. His blood work was significant for a leukocytosis with neutrophilia and an elevated D-dimer. He underwent a CTA of the chest in the emergency room to evaluate for a pulmonary embolism. The CTA of the chest had no evidence of pulmonary thromboembolic disease. However, there was unilateral ground glass opacification of the right lung with interlobular septal thickening along with volume loss of the left lung and associated elevation of the left hemidiaphragm (Figure 1). He was admitted to the medical ICU and started on broad-spectrum antibiotics. He underwent a bronchoscopy which demonstrated mucinous adenocarcinoma of the lung. His oxygen requirement was eventually weaned after multiple days in the ICU. He was discharged with follow up in the oncology clinic.
Discussion: Mucinous adenocarcinoma of the lung is the rarest type of adenocarcinoma of the lung. It is characterized as mucinous adenocarcinoma in situ, minimally invasive adenocarcinoma, and invasive mucinous adenocarcinoma. Mucinous adenocarcinoma of the lung is morphologically characterized by tall columnar cells with abundant cytoplasm that contain varying amounts of mucin. Mucus secreted by these cells can commonly be discharged as sputum. However, if airway obstruction occurs secondary to excessive mucus production, a post-obstructive pneumonia may develop. The prognosis of mucinous adenocarcinoma of the lung is poor.
Nicholas Blackstone MD1, Tammer El-Aini MD2
1Department of Internal Medicine and 2Department of Pulmonary and Critical Care, South Campus, Banner University Medical Center – Tucson, Tucson, AZ USA
References
- Liu Y, Zhang HL, Mei JZ, Guo YW, Li RJ, Wei SD, Tian F, Yang L, Wang H. Primary mucinous adenocarcinoma of the lung: A case report and review of the literature. Oncol Lett. 2017 Sep;14(3):3701-3704. [CrossRef] [PubMed]
- Marchetti A, Buttitta F, Pellegrini S, Chella A, Bertacca G, Filardo A, Tognoni V, Ferreli F, Signorini E, Angeletti CA, Bevilacqua G. Bronchioloalveolar lung carcinomas: K-ras mutations are constant events in the mucinous subtype. J Pathol. 1996 Jul;179(3):254-9. [CrossRef] [PubMed]
- Travis WD, Brambilla E, Noguchi M, Nicholson AG, Geisinger KR, Yatabe Y, Beer DG, Powell CA, Riely GJ, Van Schil PE, Garg K, Austin JH, Asamura H, Rusch VW, Hirsch FR, Scagliotti G, Mitsudomi T, Huber RM, Ishikawa Y, Jett J, Sanchez-Cespedes M, Sculier JP, Takahashi T, Tsuboi M, Vansteenkiste J, Wistuba I, Yang PC, Aberle D, Brambilla C, Flieder D, Franklin W, Gazdar A, Gould M, Hasleton P, Henderson D, Johnson B, Johnson D, Kerr K, Kuriyama K, Lee JS, Miller VA, Petersen I, Roggli V, Rosell R, Saijo N, Thunnissen E, Tsao M, Yankelewitz D. International association for the study of lung cancer/American Thoracic Society/European Respiratory Society international multidisciplinary classification of lung adenocarcinoma. J Thorac Oncol. 2011 Feb;6(2):244-85. [CrossRef] [PubMed]
- Cai D, Li H, Wang R, Li Y, Pan Y, Hu H, Zhang Y, Gong R, Pan B, Sun Y, Chen H. Comparison of clinical features, molecular alterations, and prognosis in morphological subgroups of lung invasive mucinous adenocarcinoma. Onco Targets Ther. 2014 Nov 18;7:2127-32. [CrossRef] [PubMed].
- Xie GD, Liu YR, Jiang YZ, Shao ZM. Epidemiology and survival outcomes of mucinous adenocarcinomas: A SEER population-based study. Sci Rep. 2018 Apr 17;8(1):6117. [CrossRef] [PubMed]
Cite as: Blackstone N, El-Aini T. Medical image of the month: mucinous adenocarcinoma of the lung mimicking pneumonia. Southwest J Pulm Crit Care. 2021;22(1):8-10. doi: https://doi.org/10.13175/swjpcc072-20 PDF