SWJPCC Associate Editor Featured in Albuquerque Journal
 Monday, October 25, 2021 at 9:30AM
Monday, October 25, 2021 at 9:30AM Dr. Dona Upson forwarded an article from Sunday’s edition of the Albuquerque Journal featured Michel Boivin, a SWJPCC Associate Editor, in an article titled, “Exhaustion in the ICU: Doctors reflect on state’s nearly 5,000 COVID-19 deaths” (1). Boivin and his wife Teri Heynekamp, a married couple who were many years at the University of New Mexico, shared their thoughts last week on New Mexico nearing 5,000 COVID-19 deaths (Figure 1).

Figure 1. Lovelace doctors Michel Boivin and Teri Heynekamp, a married couple, walk through the intensive care unit at Lovelace Medical Center in Albuquerque. They and other doctors shared their thoughts last week on New Mexico nearing 5,000 COVID-19 deaths. (Eddie Moore/Albuquerque Journal)
Yesterday was Day 587 of the COVID-19 pandemic in New Mexico, just another brief hospital scene amid 19 months of loneliness, fatigue and grief. “We feel exhausted,” Heynekamp said in an interview, “like a type of exhaustion that I’ve never experienced in my life.” Doctors and other health care providers say their workload has hardly let up. Even the arrival of safe, effective vaccines, some doctors say, has provided little relief, introducing a new dynamic instead — the knowledge that most of today’s COVID-19 deaths are preventable. People who weren’t fully vaccinated accounted for 96% of the deaths in a recent four-week period.
Dr. Steve McLaughlin, chairman of the Department of Emergency Medicine at the University of New Mexico School of Medicine, said hospital leaders throughout the country are trying to address burnout among their workforce and “moral injury” — a concept usually applied to refugees and soldiers in wartime. In health care, moral injury refers to the distress endured by doctors and others as they’re forced to provide less care than normal. The preventable nature of most COVID-19 deaths, some doctors say, has added to the psychological toll.
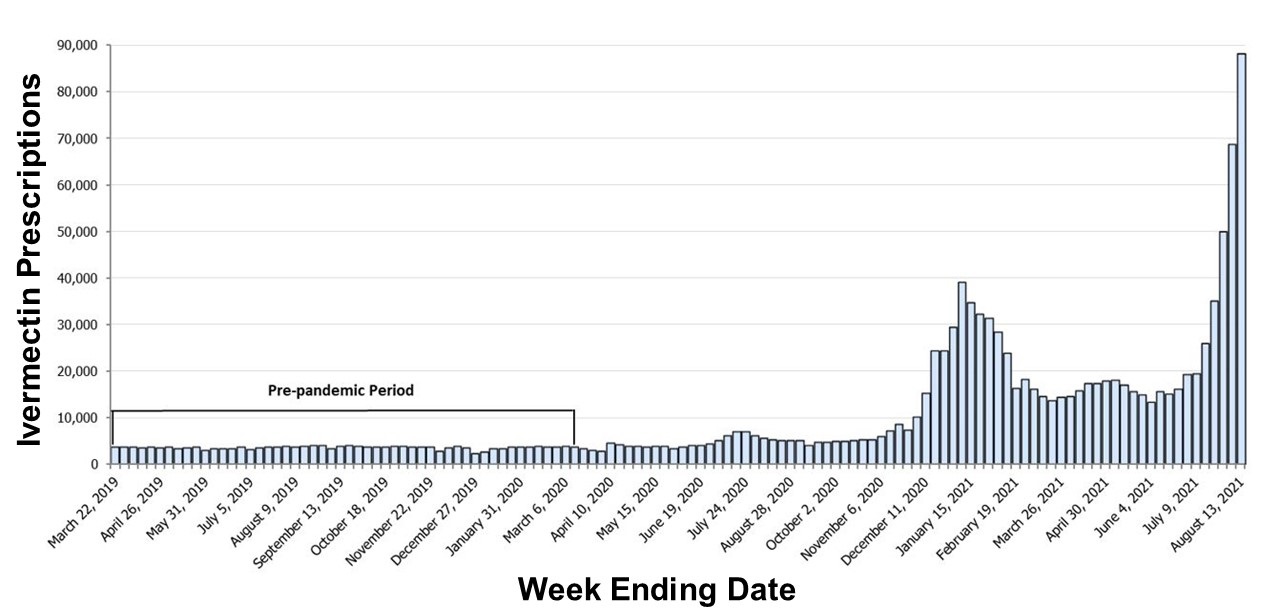
Heynekamp said they and other providers have faced patients and family members who doubt the severity of the disease. Some families ask for a specific medicine, such as ivermectin, an anti-parasite drug not approved for COVID-19 treatment. A recent ICU patient, Heynekamp said, insisted his COVID-19 infection wasn’t worse than the flu. Others want to go home against medical advice, she said, and some families reject vaccination even after a loved one dies. “There’s so much anger toward health care providers,” Heynekamp said. “There’s so much animosity. There’s so much mistrust. “We’ve never dealt with that before.” Boivin put it this way: “The way that social media rewards disinformation and spreading lies at the expense of people’s lives has been unbelievably frustrating, as well as time consuming.”
The stress on health care providers goes well beyond coronavirus infections. New Mexico has had a long-standing shortage of doctors and nurses, especially in rural areas, and fewer beds per capita than the nation as a whole. Dr. Michel Boivin, a critical care physician at Lovelace, said a key challenge now is the scarcity of space available in larger hospitals to accept patients from smaller ones. “I had a guy who needed a pacemaker,” Boivin said, “and he was sitting in a rural New Mexico hospital for a whole day with his heart barely beating.” Before the pandemic, he said, there would have been no wait for a pacemaker-related transfer.
According to Dr. Sarah Medrick at the University of New Mexico, their state has one of the highest vaccination rates in the country (Table 1) (2).
Table 1. Vaccination Rate by State (2).

They urged people to get vaccinated, wear masks indoors and wash their hands. “I feel a lot of empathy for the families who are still losing their loved ones,” McLaughlin said. “I think it’s important to remind people that the pandemic is not over, and we have to continue to focus on the things we know can keep people safe and prevent additional deaths.” As Heynekamp walked through the seventh-floor ICU at Lovelace, she noted that she had stood in many of the rooms and watched patients say goodbye, often through a video call to loved ones.
It was, she said, a lonely way to die.
References
- McKay D. Exhaustion in the ICU: Doctors reflect on state’s nearly 5,000 COVID-19 deaths. Albuquerque Journal. October 24, 2021. Available at: https://www.abqjournal.com/2440183/doctors-reflect-on-states-nearly-5000-covid19-deaths.html (accessed 10-25-21).
- COVID-19 Vaccine Statistics. Our World in Data. Available at: https://www.google.com/search?q=covid-19+vaccination+rate+in+Arizona&rlz=1C1GCEA_enUS969US969&ei=jdF2YeeSEZ-e0PEP7MCJCA&ved=0ahUKEwinjYi49OXzAhUfDzQIHWxgAgEQ4dUDCA4&uact=5&oq=covid-19+vaccination+rate+in+Arizona&gs_lcp=Cgdnd3Mtd2l6EAMyBggAEBYQHjIFCAAQhgMyBQgAEIYDOgcIABBHELADOgUIABCABEoECEEYAFCl3hJYmuUSYK_sEmgBcAJ4AIABnAGIAbgGkgEDMS42mAEAoAEByAEIwAEB&sclient=gws-wiz (accessed 10-25-21).
Cite as: Robbins RA. SWJPCC Associate Editor Featured in Albuquerque Journal. Southwest J Pulm Crit Care. 2021;23:104-6. doi: https://doi.org/10.13175/swjpcc049-21 PDF