Several sources are reporting a lawsuit filed in California alleging poor care in the state’s Medicaid program, Medi-Cal (1). The suit alleges that Medi-Cal failed to pay doctors enough to provide proper care. The suit was filed by five Latino residents on behalf of California’s 13 million lower-income residents, more than half of them Latinos. The suit alleges that "…California has created a separate and unequal system of health care, one for the insurance program with the largest proportion of Latinos (Medi-Cal), and one for the other principal insurance plans, whose recipients are disproportionately white.”
The state budget includes $107 billion in state and federal funding for Medi-Cal this year, but the spending is not enough to restore reimbursement cuts made during the Great Recession of 2008. A proposal in the U.S. Senate to repeal the Affordable Health Care law (ACA, Obamacare) could drastically reduce funding for Medicare and the individuals who can access it.
Thomas Saenz, an attorney with the Mexican American Legal Defense and Educational Fund who filed the lawsuit, said he believes it is the first time the civil rights approach has been tried in California. According to Saenz this legal approach is possible because California is one of the few states to specifically prohibit discriminatory effects in state programs.
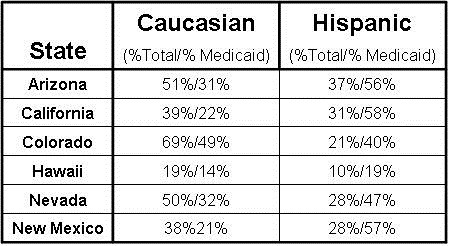
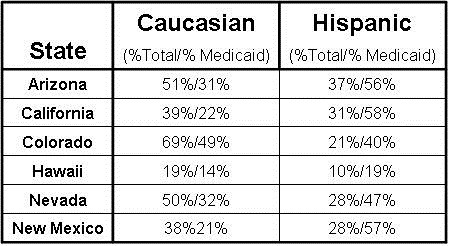
Other states in the Southwest also have disproportionately large Hispanic populations in their Medicaid programs (Table 1).
Table 1. Percent Caucasian and Hispanic total population/Medicare population by State (2,3).
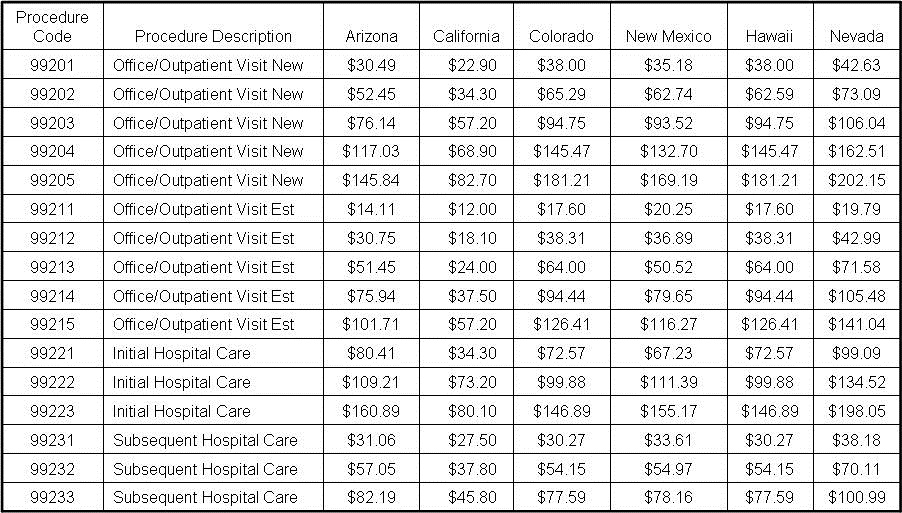
Reimbursement does appear disproportionately low in California which ranked 48th in the nation in 2015 in how much it paid hospitals, doctors and other healthcare providers for treating Medi-Cal patients, according to the Kaiser Family Foundation (4). In the Southwest the state with the highest reimbursement was Nevada (5-10). California reimbursement averaged only 47% of Nevada reimbursement for the procedures listed (Table 2).
Table 2. Medicare reimbursement for common procedures by state (4-9).
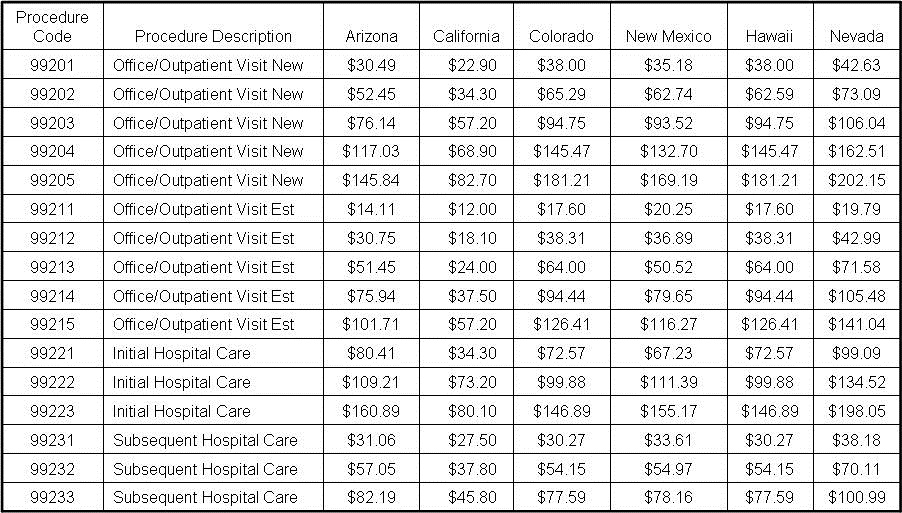
The reason for the wide differences in reimbursement rates is unclear but is likely historical dating back to cost containment programs from the 1980’s and 90’s (11). The differences do not appear to be explained by differing costs of living. None of the procedure reimbursements correlated with the cost of living in the largest city in each state (Phoenix, Los Angeles, Denver, Albuquerque, Honolulu, and Las Vegas, p>0.1, all comparisons).
The chances of the lawsuit’s success are unclear since there is no precedent. However, it seems likely that if the suit is successful, more suits will be filed since California Medi-Cal’s situation of disproportionately providing care to minorities is not unique.
Richard A. Robbins, MD
Editor, SWJPCC
References
- Thompson D. Latino plaintiffs sue California alleging poor health care. Associated Press. July 12, 2017. Available at: http://abcnews.go.com/Health/wireStory/latino-plaintiffs-sue-california-alleging-poor-health-care-48592841 (accessed 7/13/17).
- Kaiser Family Foundation. Population distribution by race/ethnicity. 2015. Available at: http://www.kff.org/other/state-indicator/distribution-by-raceethnicity/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D (accessed 7/13/17).
- Kaiser Family Foundation. Distribution of the nonelderly with Medicaid by race/ethnicity. 2015. Available at: http://www.kff.org/medicaid/state-indicator/distribution-by-raceethnicity-4/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D (accessed 7/13/17).
- Dickson V. Low Medi-Cal payments could weaken expanded coverage for undocumented children. Modern Healthcare. June 17, 2015. Available at: http://www.modernhealthcare.com/article/20150617/NEWS/150619908 (accessed 7/13/17).
- California Department of Health Care Services Medi-Cal. Medi-Cal Rates. June 15, 2017. Available at: https://files.medi-cal.ca.gov/pubsdoco/rates/rateshome.asp (accessed 7/13/17).
- Arizona Health Cost Containment System. Physician fee schedules. 2017. Available at: https://www.azahcccs.gov/PlansProviders/RatesAndBilling/FFS/Physicianrates/ (accessed 7/13/17).
- Colorado Department of Health Care Policy and Financing. Provider rates & fee schedule. June 2017. Available at: https://www.colorado.gov/pacific/hcpf/provider-rates-fee-schedule (accessed 7/13/17).
- Quest Hawai’i. Medicaid fee schedule. 2013. Available at: http://www.med-quest.us/ (accessed 7/13/17).
- Nevada Division of Health Care Financing and Policy. Fee schedules. Available at: http://dhcfp.nv.gov/Resources/Rates/FeeSchedules/ (accessed 7/13/17).
- New Mexico Human Services Department. New Mexico Medicaid fee for service CPT code fee schedule. 2017. Available at: http://www.hsd.state.nm.us/uploads/FileLinks/e7cfb008157f422597cccdc11d2034f0/7.17_CPT_Codes__2_.pdf (accessed 7/13/17).
- Tatar M, Paradise J, Grafield R. Medi-Cal managed care: an overview and key issues. Kaiser Family Foundation. Mar 02, 2016. Available at: http://www.kff.org/report-section/medi-cal-managed-care-an-overview-and-key-issues-issue-brief/ (accessed 7/13/17).
Cite as: Robbins RA. Medi-Cal blamed for poor care in lawsuit. Southwest J Pulm Crit Care. 2017;15(1):42-4. doi: https://doi.org/10.13175/swjpcc091-17 PDF
 Tuesday, November 13, 2018 at 10:45AM
Tuesday, November 13, 2018 at 10:45AM