Mortality Rate Will Likely Increase Under Senate Healthcare Bill
 Tuesday, June 27, 2017 at 8:00AM
Tuesday, June 27, 2017 at 8:00AM Today (6/27/17) an article was published in the Annals of Internal Medicine by Steffie Woolhandler and David Himmelstein from New York University on the effects of health insurance on mortality (1). The article has special significance because of pending healthcare legislation in the Senate.
The Annals article concludes that the odds of dying among the insured relative to the uninsured is 0.71 to 0.97. However, the authors acknowledge that this is a very difficult study to conduct because of the nonrandomized, observational nature of the studies and lack of a strict separation between covered and uncovered Americans. For example, many people cycle in and out of insurance diluting differences between groups.
Of course, what is needed is a randomized trial, and surprisingly, one does exist which is discussed in the Annals article (1,2). In 2008, Oregon initiated a limited expansion of its Medicaid program for about 6,000 poor, able-bodied, uninsured adults aged 19 to 64 years through a lottery to win the opportunity to apply for Medicaid and to enroll if they met eligibility requirements. Compared to uninsured adults, mortality was 13% lower in the insured. However, the trial was underpowered and the mortality differences did not reach statistical significance.
Another study mentioned was one examining the mortality rates in New York, Maine, and Arizona after expansion of Medicaid (1,3). Compared to neighboring states that did not expand Medicaid, a significant decrease in all-cause mortality in the expansion states was observed (−25.4 deaths per 100,000 population; p = 0.02; Figure 1).
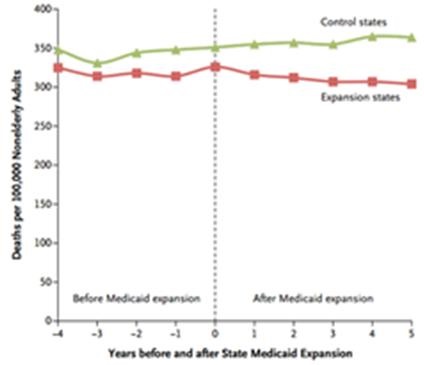
Figure 1. Unadjusted mortality and rates of Medicaid coverage among nonelderly adults before and after state Medicaid expansions (1997–2007). The vertical line represents the year during which the Medicaid expansions were implemented, meaning that year 1 was the first full year after the expansions.
Figure 1 shows roughly parallel death rates before Medicaid expansion, and a gradually widening split after Medicaid expansion. From this data, the authors calculated that Medicaid expansion to 176 adults would prevent one death per year.
On Monday (6/26/17), the Congressional Budget Office (CBO) concluded that the pending Senate healthcare bill, known as the Better Care Reconciliation Act, will result in 22 million fewer people having health insurance by 2026 (4,5). The bill would cut $772 billion in Medicaid spending and $408 billion in subsidies for individual enrollees. The net effect of these spending reductions is partially offset by $541 billion in tax cuts mostly to corporations and wealthier Americans. These numbers all approximate the effects under the similar House version of the bill that passed on May 4.
If Medicaid expansion prevents one death for each 176 enrolled (4), presumably dropping Medicaid for 176 Americans would result in one additional death per year. Given that the CBO estimates 22-23 million Americans will lose coverage under either bill, the potential increase in deaths is staggering. If either bill is passed, an increase in the death rate among the Medicaid population seems the likely consequence of the politics of reducing the Federal deficit and billions in tax cuts for corporations and the richest Americans.
Richard A. Robbins, MD
Editor, SWJPCC
References
- Woolhandler S, Himmelstein DU. The relationship of health insurance and mortality: is lack of insurance deadly? Ann Int Med. June 27, 2017. Available at: http://annals.org/aim/latest (accessed 6/27/17) [CrossRef]
- Baicker K, Taubman SL, Allen HL, Bernstein M, Gruber JH, Newhouse JP, Schneider EC, Wright BJ, Zaslavsky AM, Finkelstein AN; Oregon Health Study Group.The Oregon experiment--effects of Medicaid on clinical outcomes. N Engl J Med. 2013 May 2;368(18):1713-22. [CrossRef] [PubMed]
- Sommers BD, Baicker K, Epstein AM. Mortality and access to care among adults after state Medicaid expansions. N Engl J Med. 2012 Sep 13;367(11):1025-34. [CrossRef] [PubMed]
- Congressional Budget Office. H.R. 1628, Better Care Reconciliation Act of 2017. June 26, 2017. Available at: https://www.cbo.gov/publication/52849 (accessed 6/26/17).
- Frieden J. Senate GOP's ACA repeal bill would knock 22 million off insurance: CBO. MedPage Today. June 26, 2017. Available at: https://www.medpagetoday.com/PublicHealthPolicy/repeal-and-replace/66275?isalert=1&uun=g687171d5575R5764210u&xid=NL_breakingnews_2017-06-26 (accessed 6/26/17).
Cite as: Robbins RA. Mortality rate will likely increase under Senate healthcare bill. Southwest J Pulm Crit Care. 2017;14(6):318-9. doi: https://doi.org/10.13175/swjpcc084-17 PDF
