Richard A. Robbins, MD
Phoenix Pulmonary and Critical Care Research and Education Foundation
Gilbert, AZ USA
Abstract
The currently available evidence for the use of chronic antibiotic therapy, principally macrolides and tetracyclines, as anti-inflammatory therapy in pulmonary disorders is reviewed. Historically, treatment of a number of chronic diseases with tetracyclines showed modest benefits but reports of the successful treatment of diffuse panbronchiolitis with erythromycin stimulated research in other lung diseases as well as shifting the focus from tetracyclines to macrolides. Chronic macrolide therapy is now recommended for patients with frequent exacerbations of cystic fibrosis and COPD and considerable evidence exists for potential benefits in asthma. There is also evidence of macrolide efficacy in the prevention of obliterative bronchiolitis after lung transplantation. Small trials have suggested possible benefit of macrolides in IPF. Taken together these suggest a potential for antibiotics, particularly macrolides, in some pulmonary inflammatory disorders.
History
Based on responses to antibiotics the concept arose over 70 years ago that several common diseases might have an infectious origin. In 1949, Thomas McPherson Brown reported favorable results of tetracycline treatment for rheumatoid arthritis patients at the 7th International Congress on Rheumatic Diseases (1). It was hypothesized these effects were due to a mycoplasma infection. However, the beneficial effects of cortisone in the treatment of arthritis were described at the same meeting. The effect of tetracycline paled beside that of steroids, and the salutary effects of antibiotics on rheumatoid arthritis were largely ignored.
Acne rosacea is a common, chronic dermatologic condition, whose cause remains unknown. Tetracyclines were the first systemic drugs used in the treatment of rosacea, and have been the mainstay therapy for more than 50 years (2). More recently, sub-antimicrobial doses of tetracyclines have been shown to be effective in rosacea presumably through an anti-inflammatory effect (3). Dermatitis herpetiformis is a disease now thought to be secondary to gluten sensitivity. However, this disorder has been treated with dapsone for over 60 years despite its non-infectious origin (4).
Tetracyclines have long been used for periodontal disease with clinical benefit presumed to be from their antimicrobial properties. However, as early as 1983, Golub (5) proposed that tetracyclines might have a beneficial effect by modifying inflammation. Now the tetracyclines are thought to exert their beneficial effects by anti-inflammatory effects, anti-collagenase effects, and a reduction in bone loss (6).
In 1959 the late Neil Cherniack published a double-blind study of 67 patients with chronic bronchitis or bronchiectasis treated with tetracycline, penicillin, a combination of oleandomycin and penicillin, or placebo for 3 to 22 months (7). Patients who received tetracycline had significantly fewer lower respiratory illnesses than those treated with placebos or penicillin. The average duration of these illnesses was also shorter in patients treated with tetracycline.
The anti-inflammatory effects of the macrolides were brought to light because of their effects on an uncommon pulmonary disease, diffuse panbronchiolitis (DPB). DPB is a rare disease seen in Japan and characterized by a chronic inflammatory neutrophilic inflammation of the airways, DPB has a 5-year survival rate of just 63% but only 8% when patients’ airways became colonized with Pseudomonas aeruginosa (8). However, in the early 1980s it was discovered that chronic treatment with erythromycin resulted in dramatically improved 5-year survival to 92% (8). This improvement occurred despite a failure to eliminate the bacterial colonization and was associated with a dramatic decrease in the accumulation of airway neutrophils (8,9). Interestingly, the effect on neutrophilic inflammation was found to be a nonspecific effect of the macrolides. Other macrolides (clarithromycin, roxithromycin and azithromycin) produced a similar suppression of the neutrophilic inflammation (10).
Gradually, with a better understanding of the pathogenesis of these common disease and basic studies examining anti-inflammatory effects, the macrolides and tetracyclines were recognized as anti-inflammatories. Inflammation is proposed to play a role in the pathogenesis of a number of pulmonary disorders. The encouraging results of the above suggested that macrolides and tetracyclines might be beneficial in pulmonary inflammatory conditions. Studies have examined a number of disorders including cystic fibrosis, chronic obstructive pulmonary disease, bronchiectasis, and asthma.
Anti-inflammatory Mechanisms of Action
Macrolides and tetracyclines exert their antibacterial effects by inhibiting bacterial protein synthesis. Although the anti-inflammatory mechanisms of action of the tetracyclines and macrolides are likely multiple, one important mechanism by both is a reduction in production of a multitude of pro-inflammatory cytokines. Most of these cytokines are regulated at the transcriptional level through proteins such as nuclear factor-κβ (NF- κβ), activator protein-1 (AP-1) and/or p38 mitogen-activated protein kinases (p38 MAPK). Although the studies have varied depending on the in vitro systems examined, most have described a shortening of the half-life of pro-inflammatory cytokine mRNA usually through effect on one or more of the transcriptional control proteins (10-13).
Cystic Fibrosis
A major step in the use of antibiotics as anti-inflammatories occurred with the introduction of macrolides as adjunctive therapy in cystic fibrosis in 2003. Like diffuse panbronchiolitis, airways of cystic fibrosis patients show chronic inflammation with neutrophils which are often infected with Pseudomonas aeruginosa. Saiman et al. (14) conducted a multicenter, randomized, double-blind, placebo-controlled trial of azithromycin in cystic fibrosis patients infected with Pseudomonas. They found a reduction in exacerbations and greater weight gain in those treated with azithromycin compared to control. Following several confirming studies, cystic fibrosis patients are now commonly treated with macrolide antibiotics, especially when infected with Pseudomonas (15).
Tetracyclines have been less commonly used probably because of the staining of teeth and bone in younger, growing children. However, a recent small trial of 19 adult cystic fibrosis treated with chronic doxycycline showed an improvement in FEV1 and an increase in time to the next exacerbation compared to 20 placebo-treated controls (16). This might suggest an alternative in older patients or those at high risk for side effects from macrolides.
Non-CF Bronchiectasis
Long-term treatment with antibiotics has been recommended in patients with bronchiectasis and frequent exacerbations (17). This is based on studies showing decreased rates of exacerbations and some improvement in quality of life. It is not clear whether this effect is due to the antibacterial or anti-inflammatory properties of macrolides. In addition to Cherniak’s tetracycline trial which included bronchiectatics (7), an early MRC trial in 1957 showed that long-term twice weekly oxytetracycline over 1 year led to reduced sputum purulence, fewer days confined to bed and fewer days off work (18). Later trials in non-CF bronchiectasis have been done primarily with azithromycin and it is noted that there is an increased risk of macrolide-resistant organisms developing in these patients, as well as other risks associated with macrolide therapy including ototoxicity and QT prolongation (19).
Chronic Obstructive Pulmonary Disease
Chronic obstructive pulmonary disease (COPD) is one of the most expensive diseases to treat (20). A number of studies examining costs of COPD have shown that exacerbations, especially those resulting in hospitalization, account for the majority of costs (21,22). Although treatment with glucocorticoids, long-acting beta2-agonists, and long-acting muscarinic antagonists reduce the frequency of acute exacerbations, COPD patients receiving all three of these medications still average 1.4 acute exacerbations per year (23). Beginning in the early 2000’s there were a number of studies that reported an improvement in COPD exacerbations with macrolides (24-27). This culminated in a large, NIH-sponsored, randomized, placebo-controlled, multi-center trial demonstrating that azithromycin decreased COPD exacerbations by about 20% (28).
However, despite overwhelming data that macrolides modestly reduce COPD exacerbations and professional society recommendations for macrolide use in COPD patients at high risk for COPD exacerbations, adoption of chronic therapy with macrolides in COPD has been slow (29). The major reason appears to be concerns over side effects (29). Although azithromycin is well tolerated in the majority of patients, the drug can have serious adverse effects as noted in the trials in non-CF bronchiectasis including hearing loss and QT prolongation (29). The latter is especially concerning given that within less than one year of publication of the azithromycin NIH trial in the New England Journal of Medicine, a large trial the same reported a near 3-fold increase in mortality in patients receiving macrolides (30).
Despite early trials demonstrating efficacy in decreasing COPD exacerbations, tetracyclines have received little attention compared to macrolides. In addition to Cherniak’s study (7) there is a confirming report by Norman in 1962 (31). Tetracyclines might represent an alternative to macrolides in patients at high risk for complications from the macrolides.
Asthma
Asthma, like cystic fibrosis and COPD, is an inflammatory airway disease although usually characterized by eosinophilic inflammation. Studies suggesting macrolides might be useful as anti-inflammatories in asthma go back as far as 1970 (32). After the initial study by Itkin and Menzel (32), few studies were performed until the 2000’s. However, a 1993 study from National Jewish suggested troleandomycin might be useful as a steroid-sparing agent in children with asthma and two Japanese studies published in 1999 and 2000 with roxithromycin and clarithromycin both gave positive results in small numbers of patients (33-35).
In studies whose logic is reminiscent of Thomas McPherson Brown’s concept of mycoplasma infection in rheumatoid arthritis, Kraft et al. (36) investigated chronic chlamydia and mycoplasma infection in asthma and the response to macrolide therapy. In 2002 they reported that clarithromycin treatment increased FEV1 in asthmatics but only in those with evidence of C. pneumoniae or M. pneumoniae infection by PCR in upper and lower airway samples. Sutherland and co-workers (37) also showed improvement in airway hyper-responsiveness with clarithromycin therapy but in both PCR-positive and negative groups. The difference likely resides in identifying and chronic chlamydia and mycoplasma infection. A positive PCR does not necessarily equate to chronic infection and the serologic results from different assays are variable complicating these studies (38,39).
A number of studies have been conducted since Kraft’s investigation examining clarithromycin or azithromycin and assessing various clinical responses and inflammatory parameters in asthma (40-47). These studies have been inconsistent with some showing benefits while others did not. A Cochrane review in 2005 by Richeldi et al. (48) and a review article in 2014 by Wong et al. (49) both concluded that insufficient data existed to recommend chronic macrolide therapy in asthma.
The inconsistency in these results might be explained by the small patient numbers and because various phenotypes of asthma were included. Brusselle et al. (47) reported that azithromycin treatment significantly reduced exacerbation rates only in patients with severe neutrophilic asthma compared with placebo. However, neutrophilic asthma has been associated with increased bacterial load confusing whether benefits are due to an anti-inflammatory or an antibiotic effect (50). Furthermore, clarithromycin reduces neutrophil numbers in patients with severe asthma and it has been suggested that those patients with a neutrophilic phenotype might respond better to the anti-inflammatory effects of macrolide therapy (44,51).
A recent well-done recent study from Australia might tip the balance in favor of chronic macrolide therapy in difficult-to-control asthma. Gibson et al. (52) performed a randomized, double-blind, placebo controlled parallel group trial to determine whether oral azithromycin decreases the frequency of asthma exacerbations in 420 adults with symptomatic asthma despite current use of inhaled corticosteroid and a long-acting bronchodilator. Patients were randomly assigned to receive azithromycin 500 mg or placebo three times per week for 48 weeks. Azithromycin reduced asthma exacerbations by nearly half and significantly improved asthma-related quality of life.
Tetracyclines as anti-inflammatories in asthma have received much less attention than the macrolides. In 2008 Daoud et al. (53) reported that minocycline allowed for a reduction in steroid dose in asthmatics who were steroid-dependent. A study from India demonstrated an improvement in post bronchodilator FEV1, the FVC, and the FEF (25-75) in asthmatics treated with doxycycline (54).
Obliterative Bronchiolitis
Obliterative bronchiolitis (OB) has historically gone by a variety of terms including bronchiolitis obliterans, bronchiolitis obliterans with organizing pneumonia (BOOP) and, more recently, cryptogenic organizing pneumonia (COP) although some now separate OB as a separate entity (55). Histologically OB is very similar to diffuse panbronchiolitis, and in fact, panbronchiolitis has been grouped with OB (55). The OB histological pattern is now most commonly seen after lung transplantation or hematopoietic stem-cell transplantation (HSCT). However, OB can be seen with autoimmune disease, particularly rheumatoid arthritis; exposure to inhalational toxins such as sulfur dioxide, hydrogen sulfide, nitrogen oxides, and fly ash; and as an unusual complication following infection with adenovirus, measles virus, or mycoplasma (55).
The treatment of OB is usually corticosteroids or other immunosuppressants (55). However, since OB can result in death or decreased respiratory function, studies with adjunctive therapy or prevention of OB have been of interest. Azithromycin has resulted in improved pulmonary function in approximately 50% of lung-transplant recipients with obliterative bronchiolitis (56,57). A retrospective analysis indicated that the administration of azithromycin in patients with obliterative bronchiolitis after lung transplantation is associated with improved survival (58). Studies examining azithromycin after HSCT were done given the beneficial effects after lung transplantation. Surprisingly, the results were completely different. In a randomized clinical trial that included 465 patients, 2-year airflow decline-free survival was significantly worse for the azithromycin group than for the placebo group (59). The trial was terminated early for a significant increased risk in the azithromycin group of hematological relapses. The FDA recently issued a warning against using chronic azithromycin therapy in HSCT.
There is a paucity of data on treatment of OB with macrolides in non-transplant conditions. In 1993, Ichikawa et al. (60) used erythromycin for 3-4 months in six patients with a diagnosis of bronchiolitis obliterans OP confirmed on histological examination. All improved by the completion of therapy. However, a recent trial of azithromycin in eight patients with post-infectious OB did not produce an improvement in pulmonary function parameters (61). No studies were identified using tetracyclines as therapy in OB.
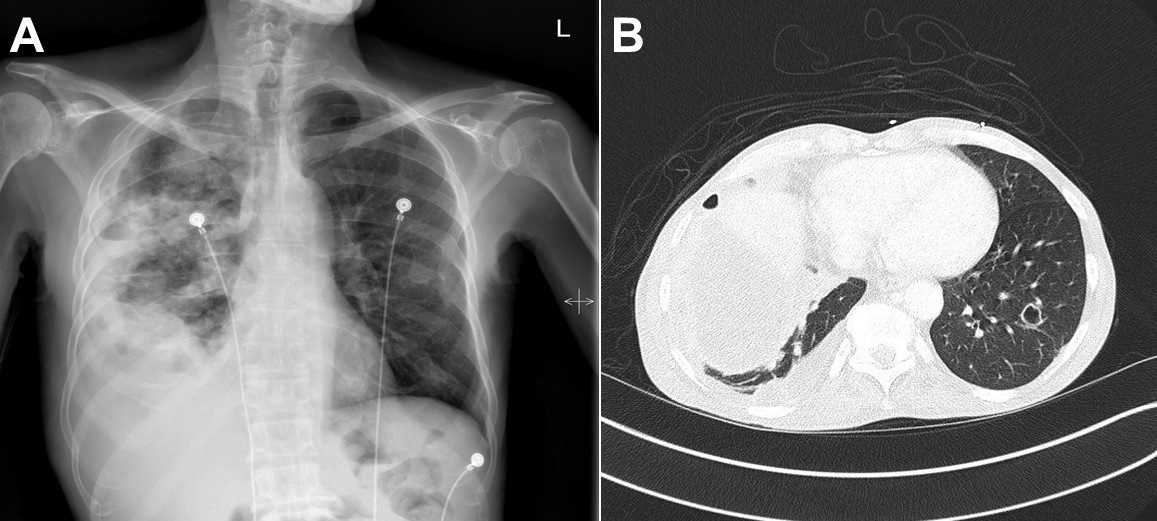
Cryptogenic Organizing Pneumonia
This entity, which was formerly known as bronchiolitis with organizing pneumonia (BOOP) can involve small airways, but also involves alveolar ducts and alveoli and can present as patchy peripheral opacities (62). It is considered an inflammatory disease which is usually very responsive to corticosteroid therapy, but may relapse when steroid therapy is withdrawn (63). There are several reports now that cryptogenic organizing pneumonia responds to treatment with macrolide and suggest that long term suppression with macrolides can avoid side effects associated with long term steroid therapy (63).
Idiopathic Pulmonary Fibrosis
Idiopathic pulmonary fibrosis (IPF) is a condition that has also been associated with neutrophils but with inflammation in the alveoli rather than the airways. With the introduction of nintedanib and pirfenidone and the realization that corticosteroids are of no benefit, the management of IPF has dramatically changed over the past decade (64). A recent publication done during the course of the shift in IPF therapy suggests that azithromycin added to conventional reduced the incidence of acute exacerbations (65). However, these retrospective results need to be interpreted with caution, since as noted above “conventional therapy” for IPF has changed profoundly. For example, many of the patients included in this study were subjected to corticosteroid therapy or other immunosuppressive agents, both of which are no longer recommended in IPF treatment (65). A similar study was performed by Kawamura et al. (66) performed from 2005-16. This single-center retrospective study of patients with IPF demonstrated that treatment of 38 consecutive patients with azithromycin (500 mg/day) for 5 days led to increased survival compared to 47 historical controls treated with a fluoroquinolone-based regimen.
A trial with minocycline in IPF was registered at clinicaltrials.gov but results were apparently never published (67). A small trial in 6 IPF patients treated with doxycycline for 24 weeks showed significant improvement in 6-minute walk time, St. George’s Respiratory Questionnaire, FVC, and quality of life compared to 6 controls (68).
Lymphangioleiomyomatosis
Lymphangioleiomyomatosis (LAM) is a rare disease that lead to progressive cystic destruction of the lungs. A recent study with doxycycline in LAM patients produced no effect upon vital capacity, gas transfer, shuttle walk distance or quality of life (69). The authors concluded that it is unlikely that doxycycline has a useful effect in LAM.
Summary
Macrolides are clinically useful in reducing exacerbations of cystic fibrosis, chronic obstructive pulmonary disease, bronchiolitis obliterans after lung transplantation, and possibly asthma. Tetracyclines might be considered as a substitute in some situations.
References
- Clark HW. Thomas McPherson Brown, M.D.: treatment of rheumatoid disease. The Arthritis Trust of America. 2000. Available at: http://arthritistrust.org/wp-content/uploads/2013/03/Thomas-McPherson-Brown-MD-Treatment-of-Rheumatoid-Disease.pdf (accessed 8/15/18).
- Sneddon IB. A clinical trial of tetracycline in rosacea. Br J Dermatol. 1966;78:649-52. [CrossRef] [PubMed]
- Valentín S, Morales A, Sánchez JL, Rivera A. Safety and efficacy of doxycycline in the treatment of rosacea. Clin Cosmet Investig Dermatol. 2009 Aug 12;2:129-40. [PubMed]
- Morgan JK, Marsden CS, Coburn JG, Mungavin JM. Dapsone in dermatitis herpetiformis. Lancet. 1955 Jun 11;268(6876):1197-1200. [CrossRef]
- Golub LM, Lee HM, Lehrer G, et al. Minocycline reduces gingival collagenolytic activity during diabetes: preliminary observations and a proposed new mechanism of action. J Periodontal Res 1983;18:516-26. [CrossRef] [PubMed]
- Paquette DW, Williams RC. Modulation of host inflammatory mediators as a treatment strategy for periodontal diseases. Periodontol 2000. 2000 Oct;24:239-52. [CrossRef] [PubMed]
- Cherniack NS, Vosti KL, Dowling HF, Lepper MH, Jackson GG. Long-term treatment of bronchlectasis and chronic bronchitis; a controlled study of the effects of tetracycline, penicillin, and an oleandomycinpenicillin mixture. AMA Arch Intern Med. 1959 Mar;103(3):345-53. [CrossRef] [PubMed]
- Kudoh S, Azuma A, Yamamoto M, et al. Improvement of survival in patients with diffuse panbronchiolitis treated with lowdose erythromycin. Am J Respir Crit Care Med. 1998;157:1829–32. [CrossRef] [PubMed]
- Oda H, Kadota J, Kohno S, Hara K. Erythromycin inhibits neutrophil chemotaxis in bronchoalveoli of diffuse panbronchiolitis. Chest. 1994 Oct;106(4):1116-23. [CrossRef] [PubMed]
- Amsden GW. Anti-inflammatory effects of macrolides—an underappreciated benefit in the treatment of community-acquired respiratory tract infections and chronic inflammatory pulmonary conditions? J Antimicrob Chemother. 2005 Jan;55(1):10-21. [CrossRef] [PubMed]
- Hoyt JC, Robbins RA. Macrolide antibiotics and pulmonary inflammation. FEMS Microbiol Lett. 2001 Nov 27;205(1):1-7. [CrossRef] [PubMed]
- Harvey RJ, Wallwork BD, Lund VJ. Anti-inflammatory effects of macrolides: applications in chronic rhinosinusitis. Immunol Allergy Clin North Am. 2009 Nov;29(4):689-703. [CrossRef] [PubMed]
- Rempe S, Hayden JM, Robbins RA, Hoyt JC. Tetracyclines and pulmonary inflammation. Endocr Metab Immune Disord Drug Targets. 2007 Dec;7(4):232-6. [CrossRef] [PubMed]
- Saiman L, Marshall BC, Mayer-Hamblett N, et al. Azithromycin in patients with cystic fibrosis chronically infected with Pseudomonas aeruginosa: a randomized controlled trial. JAMA. 2003 Oct 1;290(13):1749-56. [CrossRef] [PubMed]
- Mogayzel PJ Jr, Naureckas ET, Robinson KA, et al. Cystic fibrosis pulmonary guidelines. Chronic medications for maintenance of lung health. Am J Respir Crit Care Med. 2013 Apr 1;187(7):680-9. [CrossRef] [PubMed]
- Hill AT. Macrolides for Clinically Significant bronchiectasis in adults: who should receive this treatment? Chest. 2016 Dec;150(6):1187-93. [CrossRef] [PubMed]
- Medical Research Council. Prolonged antibiotic treatment of severe bronchiectasis; a report by a subcommittee of the Antibiotics Clinical Trials (non-tuberculous) Committee of the Medical Research Council. BMJ. 1957;2:255–9. [PubMed]
- Kelly C, Chalmers JD, Crossingham I, et al. Macrolide antibiotics for bronchiectasis. Cochrane Database Syst Rev. 2018 Mar 15;3:CD012406. [CrossRef] [PubMed]
- Xu X, Abdalla T, Bratcher PE, et al. Doxycycline improves clinical outcomes during cystic fibrosis exacerbations. Eur Respir J. 2017 Apr 5;49(4). pii: 1601102. [CrossRef] [PubMed]
- Druss BG, Marcus SC, Olfson M, Pincus HA. The most expensive medical conditions in America. Health Aff (Millwood). 2002;21:105-11. [CrossRef]
- Friedman M, Hilleman DE. Economic burden of chronic obstructive pulmonary disease. Impact of new treatment options. Pharmacoeconomics. 2001;19(3):245-54. [CrossRef] [PubMed]
- Strassels SA, Smith DH, Sullivan SD, Mahajan PS. The costs of treating COPD in the United States. Chest. 2001;119:344-52. [CrossRef] [PubMed]
- Aaron SD, Vandemheen KL, Fergusson D, et al. Tiotropium in combination with placebo, salmeterol, or fluticasone-salmeterol for treatment of chronic obstructive pulmonary disease: a randomized trial. Ann Intern Med. 2007;146:545-55. [CrossRef] [PubMed]
- Gomez J, Banos V, Simarro E, et al. Prospective, comparative study (1994-1998) of the influence of short-term prophylactic treatment with azithromycin on patients with advanced COPD. Rev Esp Quimioter. 2000;13:379-83. [PubMed]
- Suzuki T, Yanai M, Yamaya M, et al. Erythromycin and common cold in COPD. Chest 2001;120:730-3. [CrossRef] [PubMed]
- Seemungal TAR, Wilkinson TMA, Hurst JR, Perera WR, Sapsford RJ, Wedzicha JA. Long-term erythromycin therapy is associated with decreased chronic obstructive pulmonary disease exacerbations. Am J Respir Crit Care Med. 2008;178:1139-47. [CrossRef] [PubMed]
- Blasi F, Bonardi D, Aliberti S, et al. Long-term azithromycin use in patients with chronic obstructive pulmonary disease and tracheostomy. Pulm Pharmacol Ther. 2010;3:200-7. [CrossRef] [PubMed]
- Albert RK, Connett J, Bailey WC, et al. Azithromycin for prevention of exacerbations of COPD. N Engl J Med. 2011 Aug 25;365(8):689-98. [CrossRef] [PubMed]
- Taylor SP, Sellers E, Taylor BT. Azithromycin for the prevention of copd exacerbations: the good, bad, and ugly. Am J Med. 2015 Dec;128(12):1362.e1-6. [CrossRef] [PubMed]
- Ray WA, Murray KT, Hall K, Arbogast PG, Stein CM. Azithromycin and the risk of cardiovascular death. N Engl J Med. 2012 May 17;366(20):1881-90. [CrossRef] [PubMed]
- Norman PS, Hook EW, Petersdorf RG, et al. Long-term tetracycline treatment of chronic bronchitis. JAMA. 1962;179(11):833-40. [CrossRef] [PubMed]
- Itkin IH, Menzel ML. The use of macrolide antibiotic substances in the treatment of asthma. J Allergy. 1970 Mar;45(3):146-62. [PubMed]
- Kamada AK, Hill MR, Iklé DN, Brenner AM, Szefler SJ. Efficacy and safety of low-dose troleandomycin therapy in children with severe, steroid-requiring asthma. J Allergy Clin Immunol. 1993;91:873-82. [CrossRef]
- Shoji T, Yoshida S, Sakamoto H, Hasegawa H, Nakagawa H, Amayasu H. Anti-inflammatory effect of roxithromycin in patients with aspirin-intolerant asthma. Clin Exp Allergy. 1999;29:950-6. [CrossRef] [PubMed]
- Amayasu H, Yoshida S, Ebana S, et al. Clarithromycin suppresses bronchial hyperresponsiveness associated with eosinophilic inflammation in patients with asthma. Ann Allergy Asthma Immunol. 2000 Jun;84(6):594-8. [CrossRef]
- Kraft M, Cassell GH, Pak J, Martin RJ. Mycoplasma pneumoniae and Chlamydia pneumoniae in asthma: effect of clarithromycin. Chest. 2002;121:1782-8. [CrossRef] [PubMed]
- Sutherland ER, King TS, Icitovic N, et al. A trial of clarithromycin for the treatment of suboptimally controlled asthma. J Allergy Clin Immunol. 2010;126:747–53. [CrossRef] [PubMed]
- Daxboeck F, Krause R, Wenisch C. Laboratory diagnosis of Mycoplasma pneumoniae infection. Clin Microbiol Infect. 2003;9:263-73. [CrossRef] [PubMed]
- Dowell SF, Peeling RW, Boman J, et al. Standardizing Chlamydia pneumoniae assays: recommendations from the Centers for Disease Control and Prevention (USA) and the Laboratory Centre for Disease Control (Canada). Clin Infect Dis. 2001;33:492-503. [CrossRef] [PubMed]
- Kostadima E, Tsiodras S, Alexopoulos EI, et al. Clarithromycin reduces the severity of bronchial hyperresponsiveness in patients with asthma. Eur Respir J. 2004;23:714-7. [CrossRef] [PubMed]
- Hahn DL, Plane MB, Mahdi OS, Byrne GI. Secondary outcomes of a pilot randomized trial of azithromycin treatment for asthma. PLoS Clin Trials. 2006;1: e11. [CrossRef] [PubMed]
- Piacentini GL, Peroni DG, Bodini A, et al. Azithromycin reduces bronchial hyperresponsiveness and neutrophilic airway inflammation in asthmatic children: a preliminary report. Allergy Asthma Proc 2007; 28: 194–98. [CrossRef] [PubMed]
- Strunk RC, Bacharier LB, Phillips BR, et al. Azithromycin or montelukast as inhaled corticosteroid-sparing agents in moderate to-severe childhood asthma study. J Allergy Clin Immunol 2008;122:1138-44. [CrossRef] [PubMed]
- Simpson JL, Powell H, Boyle MJ, Scott RJ, Gibson PG. Clarithromycin targets neutrophilic airway inflammation in refractory asthma. Am J Respir Crit Care Med. 2008; 177:148-55. [CrossRef] [PubMed]
- Hahn DL, Grasmick M, Hetzel S, Yale S, and the AZMATICS (AZithroMycin-Asthma Trial In Community Settings) Study Group. Azithromycin for bronchial asthma in adults: an effectiveness trial. J Am Board Fam Med. 2012;25:442-59. [CrossRef] [PubMed]
- Cameron EJ, Chaudhuri R, Mair F, et al. Randomised controlled trial of azithromycin in smokers with asthma. Eur Respir J. 2013;42:1412-5. [CrossRef] [PubMed]
- Brusselle GG, Vanderstichele C, Jordens P, et al. Azithromycin for prevention of exacerbations in severe asthma (AZISAST): a multicentre randomised double-blind placebo-controlled trial. Thorax. 2013;68:322-9. [CrossRef] [PubMed]
- Richeldi L, Ferrara G, Fabbri LM, Lasserson TJ, Gibson PG. Macrolides for chronic asthma. Cochrane Database Syst Rev. 2005;4:CD002997. [CrossRef]
- Wong EH, Porter JD, Edwards MR, Johnston SL. The role of macrolides in asthma: current evidence and future directions. Lancet Respir Med. 2014 Aug;2(8):657-70. [CrossRef]
- Wood LG, Simpson JL, Hansbro PM, Gibson PG. Potentially pathogenic bacteria cultured from the sputum of stable asthmatics are associated with increased 8-isoprostane and airway neutrophilia. Free Radic Res. 2010;44:146-54. [CrossRef] [PubMed]
- Brusselle GG, Joos G. Is there a role for macrolides in severe asthma? Curr Opin Pulm Med. 2014 Jan;20(1):95-102. [CrossRef] [PubMed]
- Gibson PG, Yang IA, Upham JW, et al. Effect of azithromycin on asthma exacerbations and quality of life in adults with persistent uncontrolled asthma (AMAZES): a randomised, double-blind, placebo-controlled trial. Lancet. 2017 Aug 12;390(10095):659-68. [CrossRef]
- Daoud A, Gloria CJ, Taningco G, et al. Minocycline treatment results in reduced oral steroid requirements in adult asthma. Allergy Asthma Proc. 2008 May-Jun;29(3):286-94. [CrossRef] [PubMed]
- Bhattacharyya P, Paul R, Bhattacharjee P, et al. Long-term use of doxycycline can improve chronic asthma and possibly remodeling: the result of a pilot observation. J Asthma Allergy. 2012;5:33-7. [CrossRef] [PubMed]
- Barker AF, Bergeron A, Rom WN, Hertz MI. Obliterative bronchiolitis. N Engl J Med. 2014 May 8;370(19):1820-8. [CrossRef] [PubMed]
- Gerhardt SG, McDyer JF, Girgis RE, Conte JV, Yang SC, Orens JB. Maintenance azithromycin therapy for bronchiolitis obliterans syndrome: results of a pilot study. Am J Respir Crit Care Med. 2003;168:121-5. [CrossRef] [PubMed]
- Federica M, Nadia S, Monica M, et al. Clinical and immunological evaluation of 12-month azithromycin therapy in chronic lung allograft rejection. Clin Transplant. 2011;25:E381-9. [CrossRef] [PubMed]
- Jain R, Hachem RR, Morrell MR, et al. Azithromycin is associated with increased survival in lung transplant recipients with bronchiolitis obliterans syndrome. J Heart Lung Transplant. 2010;29:531-7. [CrossRef] [PubMed]
- Bergeron A, Chevret S, Granata A, et al. Effect of Azithromycin on Airflow Decline-Free Survival After Allogeneic Hematopoietic Stem Cell Transplant: The ALLOZITHRO Randomized Clinical Trial. JAMA. 2017;318(6):557-66. [CrossRef] [PubMed]
- Ichikawa Y, Ninomiya H, Katsuki M, et al. Low-dose/long-term erythromycin for treatment of bronchiolitis obliterans organizing pneumonia (BOOP). Kurume Med J. 1993; 40:65–7. [CrossRef] [PubMed]
- Zeynep Seda Uyan ZS, Levent Midyat L, Erkan Çakir E, et al. Azithromycin therapy in children with postinfectious bronchiolitis obliterans. Eur Respir J. 2016;48 (suppl 60):PA1602.
- Epler GR, Colby TV, McLoud TC, Carrington CB, Gaensler EA. Bronchiolitis obliterans organizing pneumonia. N Engl J Med 1985;312:152-8.
- Pathak V, Kuhn JM, Durham C, Funkhouser WK, Henke DC. Macrolide use leads to clinical and radiological improvement in patients with cryptogenic organizing pneumonia. Ann Am Thorac Soc. 2014 Jan;11(1):87-91. [CrossRef] [PubMed]
- Raghu G, Rochwerg B, Zhang Y, et al. An official ATS/ERS/JRS/ALAT clinical practice guideline: treatment of idiopathic pulmonary fibrosis. an update of the 2011 clinical practice guideline. Am J Respir Crit Care Med. 2015 Jul 15;192(2):e3-19. [CrossRef] [PubMed]
- Kuse N, Abe S, Hayashi H, et al. Long-term efficacy of macrolide treatment in idiopathic pulmonary fibrosis: a retrospective analysis. Sarcoidosis Vasc Diffuse Lung Dis. 2016;33:242-6. [PubMed]
- Kawamura K, Ichikado K, Yasuda Y, Anan K, Suga M. Azithromycin for idiopathic acute exacerbation of idiopathic pulmonary fibrosis: a retrospective single-center study. BMC Pulm Med. 2017 Jun 19;17(1):94. [CrossRef] [PubMed]
- Minocycline therapy for lung scarring in patients with idiopathic pulmonary fibrosis - a pilot study. Available at: https://clinicaltrials.gov/ct2/show/NCT00203697 (accessed 8/29/18).
- Mishra A, Bhattacharya P, Paul S, Paul R, Swarnakar S. An alternative therapy for idiopathic pulmonary fibrosis by doxycycline through matrix metalloproteinase inhibition. Lung India. 2011 Jul;28(3):174-9. [CrossRef] [PubMed]
- Chang WY, Cane JL, Kumaran M, et al. A 2-year randomised placebo-controlled trial of doxycycline for lymphangioleiomyomatosis. Eur Respir J. 2014;43:1114-23. [CrossRef] [PubMed]
Cite as: Robbins RA. Antibiotics as anti-inflammatories in pulmonary diseases. Southwest J Pulm Crit Care. 2018;17(3):97-107. doi: https://doi.org/10.13175/swjpcc104-18 PDF
 Thursday, January 24, 2019 at 8:00AM
Thursday, January 24, 2019 at 8:00AM