COPD Exacerbations: An Evidence-Based Review
 Friday, July 20, 2012 at 9:27AM
Friday, July 20, 2012 at 9:27AM Richard A. Robbins, MD
Phoenix Pulmonary and Critical Care Research and Education Foundation
Gilbert, AZ
Abstract
COPD exacerbations are a major source of COPD morbidity, mortality and cost. Exacerbations tend to become more frequent as COPD progresses with the cause assumed to be infectious in about 80% of patients. The mainstay of management is inhaled bronchodilators with judicious use of oxygen, antibiotics, corticosteroids and assisted ventilation. Recent studies have examined strategies to prevent exacerbations of COPD including use of macrolide antibiotics and self-management education.
Definition of COPD Exacerbations
There is no standard definition of COPD exacerbations. However, the workshop, “COPD: Working Towards a Greater Understanding”, proposed the following working definition in 2000: “A sustained worsening of the patient’s condition, from the stable state and beyond normal day-to-day variations, that is acute in onset and necessitates a change in regular medication in a patient with underlying COPD” (1). This seems to be the mostly commonly used definition today. Others have defined exacerbations specifically in terms of increased dyspnea, sputum production, or sputum purulence (2,3). However, exacerbations of COPD comprise a range of symptoms making specific medical complaints difficult to include in a comprehensive definition (1).
Epidemiology of COPD Exacerbations
Exacerbations reduce quality of life, speed disease progression, and increase the risk of death (4,5). Furthermore, exacerbations resulting in hospitalization account for the major cost of COPD (6). The best predictor of future exacerbations is a history of frequent exacerbations (7). As many as 50% of exacerbations are not reported to physicians and 3-16% require hospitalization (8). Hospital mortality is 3-10% and mortality of ICU admission is 15-24%. Half of the patients hospitalized will require readmission in the next 6 months (8).
Frequency of exacerbations increase with increasing severity of COPD. In a systematic review, patients with mild COPD had a mean of 0.82 exacerbations per year (9). The rates increased to 1.17, 1.61, and 2.01 in patients with moderate, severe, and very severe disease, respectively.
COPD is a lung disease that is frequently associated with other comorbid conditions. These comorbidities affect health outcomes, increase the risks of hospital admission, increase the risk of death, and account for more than 50% of use of health-care resources for COPD (10,11). The relationship of certain comorbidities with COPD is not surprising because of COPD’s connection with cigarette smoking and aging. Cigarette smoking is not only a major risk factor for COPD, but also for cardiovascular disease, osteoporosis, and lung cancer and all are more frequently seen in COPD patients (12). Aging is a major risk factor for most chronic diseases including COPD. Almost half of all COPD patients aged 65 years or over have at least three chronic medical disorders (13). Consistent with this concept, a cluster analysis indicated that age rather than FEV₁ accounted for most of the comorbidities and symptoms (14). Furthermore physical inactivity, which is frequently observed in COPD, has been linked to aging and to major comorbidities (15-17). The presence of comorbidities likely explains why clinical outcomes in COPD only weakly correlate with the FEV1 (18).
Another common denominator between COPD and its major comorbidities is systemic inflammation. Increased concentrations of circulating cytokines (tumor necrosis factor α and interleukins 6 and 8), adipokines (leptin, ghrelin), and acute-phase proteins (C-reactive protein, fibrinogen) are seen in COPD and its comorbid diseases (19). In several studies biomarkers of systemic inflammation have been observed in patients with COPD, particularly when disease is severe and during acute exacerbations (19,20). Whether these systemic markers spill over from the lungs into the systemic circulation or merely reflect the proinflammatory state is unclear (21). However, none of these systemic inflammatory markers have received generalized acceptance in predicting or diagnosing exacerbations.
Etiology of COPD Exacerbations
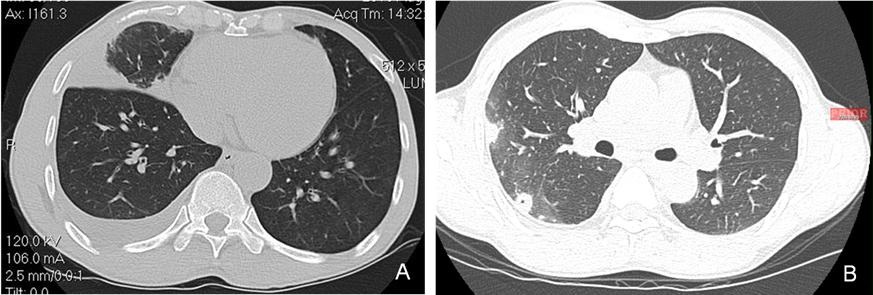
Several causes of exacerbations have been suggested for patients with COPD, including heart failure, pneumonia, pulmonary embolism, non-adherence to inhaled medication, or inhalation of irritants, such as tobacco smoke or particles (19). However, the most frequent cause cited by most is viral or bacterial infection (19). In patients admitted to hospital with COPD exacerbations, viruses, bacteria or both, were detected in 78% of cases (22). The exacerbations associated with infection were more severe than those in patients with non-infectious causes (22). However, the 80% frequency of infectious causes may be an overestimation. The accepted gold standard for the diagnosis of bacterial causes is the isolation of a potentially pathogenic bacterium by sputum culture. However, sputum cultures are neither sensitive nor specific. An additional difficulty is that a substantial proportion of patients with stable COPD have bacterial colonization (23). These include the organisms most commonly associated with exacerbations: H. influenzae, S. pneumoniae, and M. catarrhalis.
Viruses are thought to account for 15–25% of all infective exacerbations, particularly human rhinovirus, influenza, parainfluenza, and adenoviruses (19). Infection with both viruses and bacteria are seen in 25% of patients with exacerbations who are admitted to hospital (22). Viral exacerbations are strongly correlated with colds at presentation, high frequency of exacerbations, and severe respiratory symptoms during exacerbations. Experimental evidence suggests that upper respiratory tract infections can lead to lower respiratory tract inflammation and symptoms. COPD patients experimentally infected in the upper respiratory tract with rhinovirus developed lower respiratory symptoms, airflow obstruction, systemic inflammation, and inflammation in their airways (24). In addition to inducing lower respiratory inflammation and symptoms, viral infections may facilitate subsequent bacterial infection. Although viral infections are usually self-limiting, secondary bacterial infection may prolong exacerbations (24).
Gastroesophageal reflux has been suggested to play an important role in a number of respiratory diseases and has been independently associated with increased frequency of COPD exacerbations (7). Similarly, sleep-apnea has also been shown to be an independent predictor of COPD exacerbations (25).
No serum marker of bacterial or viral infection in COPD exacerbations has gained general acceptance. However, measurements of procalcitonin and C-reactive protein have been suggested as predictors of bacterial infection since both have been shown to predict results to antibiotic therapy (26,27). Increased concentrations of serum interferon-γ-inducible protein10 were useful in identifying rhinovirus infection in one study (28).
A recent publication by Bafadhel et al. (29) measured biomarkers in sputum and serum from a total of 145 COPD patients. Four distinct biologic exacerbation clusters were identified. These were bacterial-, viral-, or eosinophilic-predominant, and a fourth associated with limited changes in the inflammatory profile termed “pauciinflammatory.” Of all exacerbations, 55%, 29%, and 28% were associated with bacteria, virus, or a sputum eosinophilia. The biomarkers that best identified these clinical phenotypes were sputum IL-1β, serum CXCL10, and percentage peripheral eosinophils. Future research may establish the usefulness of these as well as other biomarkers in predicting and diagnosing infectious causes of COPD exacerbations.
Diagnostic Interventions in COPD
Clinical judgment is necessary in evaluating the need for hospital admission and which diagnostic tests need to be performed. Patients with mild exacerbations may be managed as outpatients with no diagnostic testing. Patients with more severe exacerbations may need diagnostic testing and hospitalization when appropriate.
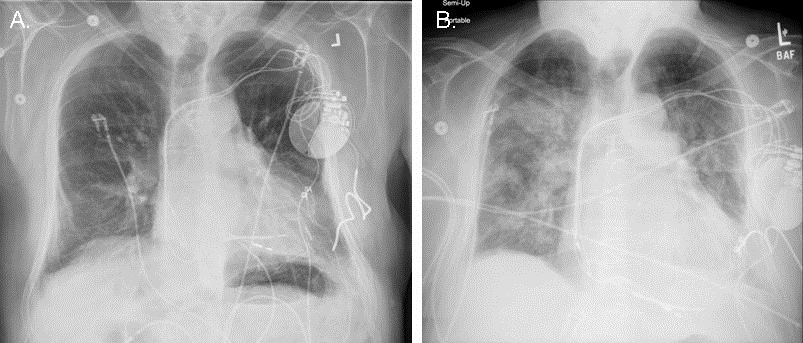
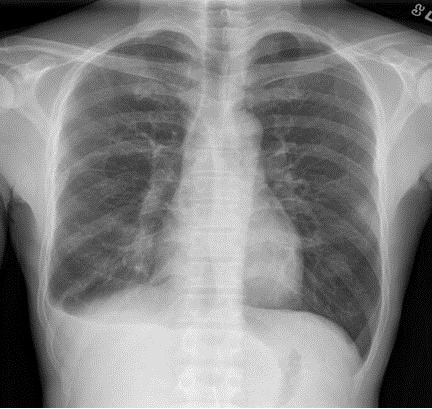
Chest x-rays have been found to be useful in evaluation of COPD exacerbations. Data from observational studies show that in 16% to 21% of the chest radiographs change patient management (30-32). Arterial blood gases are helpful in assessing the severity of an exacerbation and the degree of hypoxemia and hypercarbia. The later is particularly important in identifying patients that are likely to require hospitalization and additional ventilatory support (33). Although spirometry and peak flows may be useful in identifying an exacerbation, available evidence does not support their routine measurement to guide therapy during an exacerbation (33).
Treatment of COPD Exacerbations
Therapies for treatment of COPD exacerbations and their evidence basis are summarized in Table 1.
Table 1. Therapies for COPD exacerbations.

Oxygen. In my practice inappropriate empiric use of high doses of oxygen was becoming increasingly problematic. High doses of oxygen can result in absorption atelectasis, increased ventilation-perfusion mismatch and increased hypercarbia. The British Thoracic Society (BTS) has published guidelines that oxygen is a treatment for hypoxemia, not breathlessness or dyspnea (34). Oxygen has not been shown to affect breathlessness in nonhypoxemic patients, and therefore, empirically increasing oxygen administration for breathlessness when the oxygen saturation is satisfactory is ineffective and potentially harmful. BTS suggests oxygen should be prescribed to achieve a target saturation of 94-98% for most acutely ill patients or 88-92% for those at risk for hypercapnic respiratory failure. Hypercapnic patients at high risk for respiratory failure may usually be safely managed with oxygen saturations as low as 85-88%.
In support of the concept that empiric use of high flow oxygen may do more harm than good, Austin et al. (35) compared nontitrated high flow oxygen with titrated oxygen in the prehospital setting in COPD patients with an acute exacerbation. Those administered oxygen to a titrated oxygen saturation of 88-92% had reduced mortality, hypercapnia and respiratory acidosis compared to those treated with nontitrated oxygen at 8-10 L/min.
It appears to make little difference if oxygen is administered by nasal cannula or Venturi mask. In a study comparing patients assigned to receive oxygen through a Venturi mask or nasal prongs oxygen saturation improved to the same extent without any significant effect upon arterial carbon dioxide tension or pH (36).
Bronchodilators. The first line of treatment for a COPD exacerbation is to increase the frequency of short-acting inhaled beta 2-agonists and/or anticholinergics. However, there are only four randomized, controlled trials comparing beta 2-agonists with anticholinergics and all analyzed short-term effects (37). Overall, the available data show similar FEV1 improvement with either bronchodilator. Although use of both in combination is common, there does not appear to be strong evidence to support this approach (37,38). There is very limited data on use of long-acting beta 2-agonists (formoterol and salmeterol) or long-acting anticholinergics (tiotropium) in treatment of exacerbations of COPD.
Metered-dose inhaler (MDI) and small volume nebulizers appear to be equivalent in the acute treatment of adults with airflow obstruction (39). It is assumed that the cost of delivery is lower with MDIs due to decreased nursing or respiratory therapist time needed to administer the drugs. Spacer devices have been used with an MDI in most studies.
Thirty years ago methylxanthines, such as aminophylline, were the mainstay therapy for COPD exacerbations. However, these drugs have largely fallen out of favor. A meta-analysis on use of methylxanthines in acute COPD exacerbation did not find any evidence to support their use (40). Methylxanthines do not significantly improve FEV1 during COPD exacerbations and have a narrow therapeutic window with numerous potential side effects including nausea, vomiting, headache, arrhythmias, and seizures.
Corticosteroids. Corticosteroids significantly reduce the risk of treatment failure and length of hospital stay (41). Although the optimal dosage and length of therapy are unknown, the largest trial used methylprednisolone 125 mg intravenously every 6 hours for 72 hours (42). Two weeks of oral prednisone after intravenous therapy was as efficacious as 8 weeks (40). In a retrospective review among patients hospitalized with COPD exacerbations, oral therapy was not associated with worse outcomes compared to high-dose intravenous therapy (43).
Antibiotics. As previously mentioned, infectious etiologies may account for as many as 80% of the acute COPD exacerbations (19,22). Therefore, it is reasonable to expect that antibiotics would be efficacious. Studies going back to the 1980’s show a significant benefit of antibiotic treatment, with a success rate of 68% for the antibiotic group compared to 55% for the placebo group (2). Subsequent meta-analyses have confirmed these findings (33,44,45). Patients with more severe exacerbations are more likely to benefit from antibiotics than those with milder exacerbations. The presence of purulent sputum may be predictive of the presence of active infection and identify those patients most likely to benefit from antibiotic therapy (46).
Controversy exists regarding the choice of the newer, broad-spectrum antibiotics compared to the older, traditional antibiotics. Some studies have found significantly higher persistence or worsening of symptoms in patients treated with first-line agents (amoxicillin, cotrimoxazole, tetracyclines, or erythromycin) compared to second or third-line agents (amoxicillin/clavulanate, azithromycin, or ciprofloxacin) (47,48). On the other hand, other studies suggest that host factors rather than antibiotic choice are the primary determinants of treatment failure (49). It may be that the anti-inflammatory effects of certain antibiotics such as the macrolides or tetracyclines account for some of the variability (50,51). Recently a concern has been raised regarding macrolides causing QT prolongation and a very small, but significant, increase in cardiovascular death (52). Tetracyclines such as doxycycline may represent an alternative to the macrolides since they do not cause QT prolongation
The duration of antibiotic therapy is also controversial. However, a recent meta-analysis by El Moussaoui et al. (53) suggests that 5 days of therapy is as effective as longer durations of therapy.
Other Pharmacologic Agents. A variety of mucolytics, mucokinetics, expectorants, antiproteases, antioxidants and immunostimulants have been proposed to treat COPD exacerbations but do not have well established clinical efficacy (54). A review of mucolytic agents in acute exacerbations of COPD suggested there was no evidence that they shortened the duration of the exacerbations or improved the FEV1 (55). However, the analysis did suggest that mucolytics might improve symptoms compared to controls. In the nonacute COPD setting, a meta-analysis has found a small reduction in the number of acute exacerbations and days of illness when mucolytics were routinely used (55).
Chest Physiotherapy. During acute COPD exacerbations mechanical percussion of the chest as applied by physical/respiratory therapists is ineffective in improving symptoms or lung function, although it may increase the amount of sputum expectorated (38,56). Furthermore, there may be a transient worsening in FEV1 after chest percussion (38).
Noninvasive Positive-Pressure Ventilation (NIPPV). Noninvasive positive pressure ventilation (NIPPV) is probably the largest therapeutic advance in treating COPD exacerbations in the past 20 years. Meta-analysis has found not only a reduction in the need for intubation and mechanical ventilation with NIPPV, but also a reduction in the risk of death (57). Patients hospitalized for exacerbations of COPD with rapid clinical deterioration should be considered candidates for NIPPV. However, there are no standardized criteria to predict which patients will benefit. Therefore, careful observation, usually in the intensive care unit, is necessary should NIPPV fail.
Heliox. Helium is a low density inert gas that in combination with oxygen (heliox) has been used as an additive treatment in upper airway obstructions and other causes of respiratory failure. The rationale for its use during COPD exacerbations is to diminish respiratory effort, peak pressure, and intrinsic positive end expiratory pressure. A meta-analysis in 2002 evaluated the limited literature on the use of heliox in acute COPD exacerbations and concluded that there is insufficient data to support its use (58). A recent randomized trial failed to show heliox reduced intubation rates, duration of noninvasive ventilation, length of stay, complications or 28-day mortality (59). Furthermore, heliox has the disadvantage of coming in fixed concentrations of oxygen sometimes making its use problematic especially in hypercarbic patients.
Reduction of COPD Exacerbations
Continuous therapies for reduction of COPD exacerbations are shown in Table 2.
Table 2. Continuous therapies for reduction of COPD exacerbations.

Bronchodilators. Many of the therapies that treat COPD exacerbations have been tested to determine if chronic use might prevent exacerbations. The best evidence is for the long-acting bronchodilators. Two large randomized controlled trials have confirmed that a combination of a long-acting beta agonist (salmeterol) with an inhaled corticosteroid (fluticasone) or a long-acting anticholinergic (tiotropium) reduce exacerbations (60,61). Both appear to appear to be similarly efficacious in exacerbation reduction (62).
Research is being done with several new bronchodilators to treat COPD. Roflumilast, an oral specific phosphodiesterase 4 inhibitor, reduced the frequency of exacerbations by 17% in patients with severe or very severe COPD (63). Reductions are also seen with the addition of roflumilast to salmeterol or tiotropium (64). Several new, once-daily, long-acting beta-agonists and anticholinergics are under development and being tested alone or in combination. Indacaterol, a once daily beta-agonist, is the first of these once daily beta-agonists to become clinically available. It is anticipated that these will also reduce exacerbations similar to salmeterol/fluticasone or tiotropium.
Since both long-acting anticholinergics and long-acting beta-agonists/inhaled corticosteroids reduce exacerbations, it is logical that a combination might be additive in reducing exacerbations of COPD. However, a recent study suggests that addition of salmeterol/fluticasone to tiotropium was ineffective compared to tiotropium alone in reducing exacerbations although FEV1 and albuterol use were improved (65).
Inhaled corticosteroids. Addition of inhaled corticosteroids to long-acting bronchodilators in COPD is controversial. A recent meta-analysis by Spencer et al. (66) suggests that there was no reduction in exacerbations with addition of an inhaled corticosteroid to a long-acting beta-agonist. Furthermore, addition of corticosteroids was associated with a higher incidence of pneumonia. On the other hand, a retrospective, observational study suggested that the use of inhaled corticosteroids prior to a COPD exacerbation resulted in reduced mortality (67). In elderly COPD patients without a history of an exacerbation addition of inhaled corticosteroids was not associated with improved outcomes (68). This suggests that if inhaled corticosteroids are efficacious, they may only be efficacious in patients with a history of exacerbations.
Antibiotics. Continuous treatment with some antibiotics, particularly macrolides, reduces exacerbations. A randomized controlled trial with erythromycin reduced exacerbations by 35% compared to placebo (69). In a more recent study, treatment with azithromycin for one year lowered exacerbations by 27% (70). Although the mechanism(s) accounting for the reduction in exacerbations is unknown, current concepts suggest the reduction is likely secondary to the macrolides’ anti-inflammatory properties. However, concern has been raised about a very small, but significant, increase in QT prolongation and cardiovascular deaths with azithromycin (52). In addition, the recent trial with azithromycin raised the concern of hearing loss which occurred in 25% of patients treated with azithromycin compared to 20% of control (70). An alternative to the macrolides may be tetracyclines such as doxycycline, which also possess anti-inflammatory properties but do not lengthen QT intervals nor cause hearing loss (50).
Immunizations. Until recently, the only pneumococcal vaccine approved for use in adults in the United States and Europe was the 23-valent pneumococcal polysaccharide vaccine (PPSV23). This is despite no randomized, controlled trial of the vaccine showing a reduction in clinical outcomes (71). Recently a 7-valent diphtheria-conjugated pneumococcal vaccine has been approved for use in adults. This conjugated vaccine induces greater serotype-specific immunoglobulin G (IgG) and functional antibody than does PPSV23 for up to 2 years after vaccination (72). Whether these increases in surrogate markers will translate into lower rates of COPD exacerbations is unknown.
It appears, from the limited number of studies performed, that influenza vaccine reduces exacerbations in COPD patients (73). The effect appears to be due to a reduction in exacerbations occurring three or more weeks after vaccination due to influenza. There is a mild increase in transient local adverse effects with influenza vaccination, but no evidence that vaccination increases exacerbations immediately after administration.
Other approaches. Pulmonary rehabilitation and self-management education programs reduce hospitalization for COPD exacerbations (74, 75). A recent study found increased mortality with COPD self-management education (76) but this was not confirmed by meta-analysis (75). Lung volume reduction surgery, an approach to severe COPD, was surprisingly found to reduce exacerbation frequency (77). The cause of the reduction is unknown but may reflect the benefits of reducing hyperinflation. A specific effect of long-term oxygen in appropriate patients on reducing exacerbations has not been demonstrated. However, there is evidence that underuse of long-term oxygen therapy results in increased hospital admissions (78). Vitamin D levels have been found to be reduced in some patients with COPD. However, treatment with vitamin D did not improve exacerbation rates except those with severe vitamin D deficiency (serum 25-[OH]D levels <10 ng/mL) (79).
Clinical Approaches
Outpatient. Based on the available evidence, my approach was to prescribe antibiotics and prednisone for home use during an exacerbation to most patients with severe or very severe COPD (FEV1 < 50% predicted) and patients with moderate COPD who had been hospitalized or had frequent exacerbations. Most severe and very severe COPD patients were also treated with long-acting bronchodilators and an albuterol rescue inhaler. Many were treated with a combination of both a long-acting beta agonist (salmeterol or formoterol) with an inhaled corticosteroid and a long-acting anticholinergic. Patients with mild exacerbations were treated as outpatients with antibiotics (usually doxycycline) and oral prednisone. Prednisone was given as a fixed dose (usually 15 mg/day) for 7-14 days since tapering with short-term use is unnecessary (80). Some patients with frequent exacerbations were prescribed chronic doxycycline therapy in hopes of reducing exacerbations. Most received pulmonary rehabilitation and therapy for smoking cessation if needed.
It is usually appropriate to initiate discussions about end of life planning with a COPD patient as an outpatient (81). Autonomy of the patient is the predominant ethical principle that drives end-of-life care. These discussions should prepare patients with advanced COPD for a life-threatening exacerbation of their chronic disease. Discussions should include ICU admission and intubation and mechanical ventilation using data where appropriate to assist in the decision. Pulmonary rehabilitation provides an important opportunity to assist advance care planning for patients with moderate-to-severe COPD. Patients with COPD sometimes qualify for formal hospice services, especially when they are having repeated exacerbations and poor clinical function. Opportunities for hospice care are frequently neglected for patients coming to the end of life with COPD. Morphine is the drug of choice for the relief of dyspnea and in selected patients chronic positive pressure ventilation may be used (82).
Inpatient. My rationale was that if a patient was sick enough to be in the hospital, he was sick enough to receive bronchodilators, antibiotics, and corticosteroids. Chest x-rays and arterial blood gases were routinely performed on hospitalized patients. Those with hypercarbia and respiratory acidosis were usually admitted to the ICU and especially those with an exacerbation sufficiently severe to require noninvasive positive pressure ventilation. Oxygen was titrated to maintain the SpO2 at 88-92%, and if severe respiratory acidosis was present, oxygen was titrated to a SpO2 of 85-88%. Albuterol by MDI was used as often as needed to control symptoms, sometimes as often as every 1-2 hours with careful monitoring. Ipratropium by MDI was added if the patients were not receiving tiotropium. If the patients were taking long-acting bronchodilators as outpatients, these were continued during inpatient hospitalization. Doxycycline was used as an antibiotic in the absence of culture evidence or x-ray evidence to choose an alternative. Corticosteroids were given as methylprednisolone 125 mg IV every 6 hours for 3 days and then oral prednisone for another 2 weeks. Rarely, methylxanthines were added in those very severe patients who failed to clinically improve in 1-3 days. Those who were not on long-acting bronchodilators were started on one or both prior to discharge to reduce the number of future exacerbations. Patients were followed up in the outpatient clinic about 2-3 weeks after hospital discharge.
Conclusions
COPD exacerbations are common and can often be managed as outpatients with careful planning and education in self-management. Communication between the patient and physician regarding end of life planning is useful in planning future care during a severe exacerbation. Most patients can be managed with inhaled bronchodilators, antibiotics and corticosteroids. Titration of oxygen or administration of NIPPV usually requires hospitalization, especially in hypercarbic patients.
References
- Rodriguez-Roisin R. Toward a consensus definition for copd exacerbations. Chest 2000;117:398S-401S.
- Anthonisen NR, Manfreda J, Warren CP Hershfield ES, Harding GK, Nelson NA. Antibiotic therapy in exacerbations of chronic obstructive pulmonary disease. Ann Intern Med 1987;106:196-204.
- British Thoracic Society. BTS guidelines for the management of chronic obstructive pulmonary disease. Thorax 1997;52:S1-S28.
- Doll H, Miravitlles M. Health-related QOL in acute exacerbations of chronic bronchitis and chronic obstructive pulmonary disease: a review of the literature. Pharmacoeconomics 2005;23:345-63.
- Soler-Cataluna JJ, Martinez-Garcia MA, Roman SP, Salcedo E, Navarro M, Ochando R. Severe acute exacerbations and mortality in patients with chronic obstructive pulmonary disease. Thorax 2005;60:925-31.
- Hilleman DE, Dewan N, Malesker M, Friedman M. Pharmacoeconomic evaluation of COPD. Chest 2000;118:1278-85.
- Hurst JR, Vestbo J, Anzueto A, Locantore N, Müllerova H, Tal-Singer R, Miller B, Lomas DA, Agusti A, Macnee W, Calverley P, Rennard S, Wouters EF, Wedzicha JA; Evaluation of COPD Longitudinally to Identify Predictive Surrogate Endpoints (ECLIPSE) Investigators.. Susceptibility to exacerbation in chronic obstructive pulmonary disease. N Engl J Med 2010;363:1128-38.
- Soto FJ, Varkey B. Evidence-based approach to acute exacerbations of COPD. Curr Opin Pulm Med 2003;9:117-24.
- Hoogendoorn M, Feenstra TL, Hoogenveen RT, Al M, Mölken MR. Association between lung function and exacerbation frequency in patients with COPD. Int J Chron Obstruct Pulmon Dis 2010;5:435-44.
- Mannino DM, Thorn D, Swensen A, Holguin F. Prevalence and outcomes of diabetes, hypertension and cardiovascular disease in COPD. Eur Respir J 2008; 32: 962-9.
- Sin DD, Anthonisen NR, Soriano JB, Agusti AG. Mortality in COPD: role of comorbidities. Eur Respir J 2006; 28: 1245-57.
- Edwards R. The problem of tobacco smoking. BMJ 2004;328:217-19.
- Boyd CM, Darer J, Boult C, Fried LP, Boult L, Wu AW. Clinical practice guidelines and quality of care for older patients with multiple comorbid: implications for pay for performance. JAMA 2005;294:716-24.
- Burgel PR, Paillasseur JL, Caillaud D, Tillie-Leblond I, Chanez P, Escamilla R, Court-Fortune I, Perez T, Carré P, Roche N; Initiatives BPCO Scientific Committee. Clinical COPD phenotypes: a novel approach using principal component and cluster analyses. Eur Respir J 2010; 36: 531-39.
- Pitta F, Troosters T, Spruit MA, Probst VS, Decramer M, Gosselink R. Characteristics of physical activities in daily life in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2005;171:972-77.
- Booth FW, Gordon SE, Carlson CJ, Hamilton MT. Waging war on modern chronic diseases: primary prevention through exercise biology. J Appl Physiol 2000;88:774-87.
- Heath GW. Physical activity transitions and chronic disease. Am J Lifestyle Med 2009;3:27S-31S.
- Celli BR, Cote CG, Marin JM, Casanova C, Montes de Oca M, Mendez RA, Pinto Plata V, Cabral HJ. The body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary disease. N Engl J Med 2004;350:1005-12.
- Decramer M, Janssens W, Miravitlles M. Chronic obstructive pulmonary disease. Lancet 2012;349:1341-51.
- Broekhuizen R, Wouters EF, Creutzberg EC, et al. Raised CRP levels mark metabolic and functional impairment in advanced COPD. Thorax 2006;61:17-22.
- Sinden NJ, Stockley RA. Systemic inflammation and comorbidity in COPD: a result of ‘overspill’ of inflammatory mediators from the lungs? Review of the evidence. Thorax 2010;65:930-6.
- Papi A, Bellettato CM, Braccioni F, Romagnoli M, Casolari P, Caramori G, Fabbri LM, Johnston SL. Infections and airway inflammation in chronic obstructive pulmonary disease severe exacerbations. Am J Respir Crit Care Med 2006;173:1114-21.
- Monso E, Ruiz J, Rosell A, Manterola J, Fiz J, Morera J, Ausina V. Bacterial infection in chronic obstructive pulmonary disease. A study of stable and exacerbated outpatients using the protected specimen brush. Am J Respir Crit Care Med 1995;152:1316-20.
- Mallia P, Message SD, Gielen V, Contoli M, Gray K, Kebadze T, Aniscenko J, Laza-Stanca V, Edwards MR, Slater L, Papi A, Stanciu LA, Kon OM, Johnson M, Johnston SL. Experimental Rhinovirus infection as a human model of chronic obstructive pulmonary disease exacerbation. Am J Respir Crit Care Med 2011;183:734-42.
- Marin JM, Soriano JB, Carrizo SJ, Boldova A, Celli BR. Outcomes in patients with chronic obstructive pulmonary disease and obstructive sleep apnea: the overlap syndrome. Am J Respir Crit Care Med 2010;182:325-31.
- Stolz D, Christ-Crain M, Bingisser R, Leuppi J, Miedinger D, Müller C, Huber P, Müller B, Tamm M. Antibiotic treatment of exacerbations of COPD: a randomized, controlled trial comparing procalcitonin-guidance with standard therapy. Chest 2007;131:9-19.
- Daniels JM, Schoorl M, Snijders D, Knol DL, Lutter R, Jansen HM, Boersma WG. Procalcitonin vs C-reactive protein as predictive markers of response to antibiotic therapy in acute exacerbations of COPD. Chest 2010;138:1108-15.
- Quint JK, Donaldson GC, Goldring JJ, Baghai-Ravary R, Hurst JR, Wedzicha JA. Serum IP-10 as a biomarker of human rhinovirus infection at exacerbation of COPD. Chest 2010;137:812-22.
- Bafadhel M, McKenna S, Terry S, Mistry V, Reid C, Haldar P, McCormick M, et al. Acute exacerbations of chronic obstructive pulmonary disease: identification of biologic clusters and their biomarkers. Am J Respir Crit Care Med 2011;184:662-71.
- Emerman CL, Cydulka RK. Evaluation of high-yield criteria for chest radiography in acute exacerbation of chronic obstructive pulmonary disease. Ann Emerg Med 1993;22:680-4.
- Sherman S, Skoney JA, Raviskrishnan KP. Routine chest radiographs in exacerbations of chronic obstructive pulmonary disease: diagnostic value. Arch Intern Med 1989;149:2493-6.
- Tsai TW, Gallagher EJ, Lombardi G, Gennis P, Carter W. Guidelines for the selective ordering of admission chest radiography in adult obstructive airway disease. Ann Emerg Med 1993;22:1854-8.
- McCrory DC, Brown C, Gelfand SE, Bach PB. Management of acute exacerbations of COPD: a summary and appraisal of published evidence. Chest 2001;119:1190-1209.
- O’Driscoll BR, Howard LS, Davison AG. BTS guidelines for emergency oxygen use in adult patients. Thorax 2008;63 (Suppl VI):vi1-vi68.
- Austin MA, Wills KE, Blizzard L, Walters EH, Wood-Baker R. Effect of high flow oxygen on mortality in chronic obstructive pulmonary disease patients in prehospital setting: randomized controlled trial. BMJ 2010;341:c5462.
- Agusti AG, Carrera M, Barbe F, Muñoz A, Togores B. Oxygen therapy during exacerbations of chronic obstructive pulmonary disease. Eur Respir J 1999;14:934-939.
- McCrory DC, Brown CD. Inhaled short-acting beta2-agonists versus ipratropium for acute exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2001;(2):CD002984.
- Snow V, Lascher S, Mottur-Pilson C. Evidence base for management of acute exacerbations of chronic obstructive pulmonary disease. Ann Intern Med 2001;134:595–9.
- Turner MO, Patel A, Ginsburg S, FitzGerald JM. Bronchodilator delivery in acute airflow obstruction. A meta-analysis. Arch Intern Med 1997;157:1736-44.
- Barr RG, Rowe BH, Camargo CA, Methylxanthines for exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2003;(2):CD002168.
- Quon BS, Gen WQ, Sin DD. Contemporary management of acute exacerbations of COPD: a systematic review and meta-analysis. Chest 2008;133:156-66.
- Niewoehner DE, Erbland ML, Deupree RH, Collins D, Gross NJ, Light RW, Anderson P, Morgan NA. Effect of systemic glucocorticoids on exacerbations of chronic obstructive pulmonary disease. N Engl J Med 1999; 340:1941-7.
- Lindenauer PK, Pekow PS, Lahti, MC. Lee Y, Benjamin EM, Rothberg MB. Association of corticosteroid dose and route of administration with risk of treatment failure in acute exacerbation of chronic obstructive pulmonary disease. JAMA 2010;303:2359-67.
- Saint S, Bent S, Vittinghoff E, Grady D. Antibiotics in chronic obstructive pulmonary disease exacerbations: a meta-analysis. JAMA 1995;273:957-60.
- Ram FS, Rodriguez-Roisin R, Granados-Navarrete A, et al. Antibiotics for exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2006;2:CD004403.
- Stockley RA, O’Brien C, Pye A, Hill SL. Relation of sputum color to nature and outpatient management of acute exacerbations of COPD. Chest 2000;117:1638-45.
- Adams SG, Melo J, Luther M, Anzueto A. Antibiotics are associated with lower relapse rates in outpatients with acute exacerbations of COPD. Chest 2000;117:1345-52.
- Destache CJ, Dewan N, O’Donohue WJ, Campbell JC, Angelillo VA. Clinical and economic considerations in the treatment of acute exacerbations of chronic bronchitis. J Antimicrob Chemother 1999;43:107-13.
- Dewan NA, Rafique S, Kanwar B, Satpathy H, Ryschon K, Tillotson GS, Niederman MS. Acute exacerbation of COPD: factors associated with poor treatment outcome. Chest 2000;117:662-71.
- Rempe S, Hayden JM, Robbins RA, Hoyt JC. Tetracyclines and pulmonary inflammation. Endocr Metab Immune Disord Drug Targets 2007;7:232-6.
- Attenburg J, de Graaff CS, van der Werf TS, Boersma WG. Immunomodulatory effects of macrolide antibiotics-part 1: biological mechanisms. Respiration 2011;81:67-74.
- Ray WA, Murray KT, Hall K, Arbogast PG, Stein CM. Azithromycin and the risk of cardiovascular death. N Engl J Med 2012;366:1881-90.
- El Moussaoui R, Roede BM, Speelman P, Bresser P, Prins JM, Bossuyt PM. Short-course antibiotic treatment in acute exacerbations of chronic bronchitis and COPD: a meta-analysis of double-blind studies. Thorax 2008;63:415-22.
- Jones KL, Robbins RA. Alternative therapies for chronic bronchitis. Am J Med Sci 1999;318:96-8.
- Poole P, Black PN. Mucolytic agents for chronic bronchitis or chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2010;(2):CD001287.
- Cross J, Elender F, Barton G, Clark A, Shepstone L, Blyth A, Bachmann M, Harvey I, MATREX Research Group. A randomized, controlled equivalence trial to determine the effectiveness and cost-utility of manual chest physiotherapy techniques in the management of exacerbations of chronic obstructive pulmonary disease (MATREX). Health Technol Assess 2010;14:1-147.
- Ram FS, Picot J, Lightowler J, Wedzicha JA. Non-invasive positive pressure ventilation for treatment of respiratory failure due to exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2004; 3: CD004104.
- Rodrigo G, Pollack C, Rodrigo C, Rowe B. Heliox for treatment of exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2002, (2):CD003571.
- Maggiore SM, Richard JC, Abroug F, Diehl JL, Antonelli M, Sauder P, Mancebo J, Ferrer M, Lellouche F, Lecourt L, Beduneau G, Brochard L. A multicenter, randomized trial of noninvasive ventilation with helium-oxygen mixture in exacerbations of chronic obstructive pulmonary disease. Crit Care Med 2010;38:145-61.
- Calverley PM, Anderson JA, Celli B, Ferguson GT, Jenkins C, Jones PW, Yates JC, Vestbo J; TORCH investigators. Salmeterol and fluticasone propionate and survival in chronic obstructive pulmonary disease. N Engl J Med 2007;356:775-89.
- Tashkin DP, Celli B, Senn S, Ferguson GT, Jenkins C, Jones PW, Yates JC, Vestbo J; TORCH investigators. A 4-year trial of tiotropium in chronic obstructive pulmonary disease. N Engl J Med 2008;359:1543-54.
- Wedzicha JA, Calverley P, Seemungal T, Hagan G, Ansari Z, Stockley RA; INSPIRE Investigators. The prevention of chronic obstructive pulmonary disease exacerbations by salmeterol/fluticasone propionate or tiotropium bromide. Am J Respir Crit Care Med 2008;177:19-26.
- Calverley PM, Rabe KF, Goehring UM, Kristiansen S, Fabbri LM, Martinez FJ; M2-124 and M2-125 study groups. Roflumilast in symptomatic chronic obstructive pulmonary disease: two randomised clinical trials. Lancet 2009;374:685-94.
- Fabbri LM, Calverley PM, Izquierdo-Alonso JL, Bundschuh DS, Brose M, Martinez FJ, Rabe KF; M2-127 and M2-128 study groups. Roflumilast in moderate-to-severe chronic obstructive pulmonary disease treated with longacting bronchodilators: two randomised clinical trials. Lancet 2009;374:695-703.
- Hanania NA, Crater GD, Morris AN, Emmett AH, O'Dell DM, Niewoehner DE.Benefits of adding fluticasone propionate/salmeterol to tiotropium in moderate to severe COPD. Respir Med 2012;106:91-101.
- Spencer S, Karner C, Cates CJ, Evans DJ. Inhaled corticosteroids versus long-acting beta(2)-agonists for chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2011;(12):CD007033.
- Chen D, Restrepo MI, Fine MJ, Pugh MJ, Anzueto A, Metersky ML, Nakashima B, Good C, Mortensen EM. Observational study of inhaled corticosteroids on outcomes for COPD patients with pneumonia. Am J Respir Crit Care Med 2011;184:312-6.
- Chen S, Paluschinat CA, Wu N, Fraser K Boulanger L. Economic impact of using inhaled corticosteroids without prior exacerbation among elderly patients with chronic obstructive pulmonary disorder. J Med Econ 2011;14: 458-62.
- Seemungal TA, Wilkinson TM, Hurst JR, Perera WR, Sapsford RJ, Wedzicha JA. Long-term erythromycin therapy is associated with decreased chronic obstructive pulmonary disease exacerbations. Am J Respir Crit Care Med 2008;178:1139-47.
- Albert RK, Connett J, Bailey WC, Casaburi R, Cooper JA Jr, Criner GJ, Curtis JL, Dransfield MT, Han MK, Lazarus SC, Make B, Marchetti N, Martinez FJ, Madinger NE, McEvoy C, Niewoehner DE, Porsasz J, Price CS, Reilly J, Scanlon PD, Sciurba FC, Scharf SM, Washko GR, Woodruff PG, Anthonisen NR; COPD Clinical Research Network. COPD Clinical Research Network. Azithromycin for prevention of exacerbations of COPD. N Engl J Med 2011; 365:689-98.
- Walters JA, Smith S, Poole P, Granger RH, Wood-Baker R. Injectable vaccines for preventing pneumococcal infection in patients with chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2010; CD001390.
- Dransfield MT, Harnden S, Burton RL, Albert RK, Bailey WC, Casaburi R, Connett J, Cooper JA, Criner GJ, Curtis JL, Han MK, Make B, Marchetti N, Martinez FJ, McEvoy C, Nahm MH, Niewoehner DE, Porszasz J, Reilly J, Scanlon PD, Scharf SM, Sciurba FC, Washko GR, Woodruff PG, Lazarus SC; for the NIH COPD Clinical Research Network.Long-term comparative immunogenicity of protein conjugate and free polysaccharide pneumococcal vaccines in chronic obstructive pulmonary disease. Clin Infect Dis. 2012 Jun 19. [Epub ahead of print] (accessed 6/25/12).
- Poole PJ, Chacko E, Wood-Baker RW, Cates CJ. Influenza vaccine for patients with chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2006;(1):CD002733.
- Casaburi R, ZuWallack R. Pulmonary rehabilitation for management of chronic obstructive pulmonary disease. N Engl J Med 2009;360:1329-35.
- Hurley J, Gerkin RD, Fahy B, Robbins RA. Meta-analysis of self-management education for patients with chronic obstructive pulmonary disease. Southwest J Pulm Crit Care 2012;4:194-202.
- Fan VS, Gaziano JM, Lew R, et al. A comprehensive care management program to prevent chronic obstructive pulmonary disease hospitalizations: a randomized, controlled trial. Ann Intern Med 2012;156:673-83.
- Washko GR, Fan VS, Ramsey SD, Mohsenifar Z, Martinez F, Make BJ, Sciurba FC, Criner GJ, Minai O, Decamp MM, Reilly JJ, National Emphysema Treatment Trial Research Group. The effect of lung volume reduction surgery on chronic obstructive pulmonary disease exacerbations. Am J Respir Crit Care Med 2008;177:164-9.
- Garcia-Aymerich J, Monsó E, Marrades RM, Escarrabill J, Félez MA, Sunyer J, Antó JM, EFRAM Investigators. Risk factors for hospitalization for a chronic obstructive pulmonary disease exacerbation. EFRAM study. Am J Respir Crit Care Med 2001;164:1002-7.
- Lehouck A, Mathieu C, Carremans C, Baeke F, Verhaegen J, Van Eldere J, Decallonne B, Bouillon R, Decramer M, Janssens W.High doses of vitamin D to reduce exacerbations in chronic obstructive pulmonary disease: a randomized trial. Ann Intern Med 2012;156:105-14.
- O'Driscoll BR, Kalra S, Wilson M, Pickering CA, Carroll KB, Woodcock AA. Double-blind trial of steroid tapering in acute asthma. Lancet 1993;341:324-7
- Celli BR, MacNee W; ATS/ERS Task Force. Standards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paper. Eur Respir J 2004;23:932-46.
- Ambrosino N, Simonds A. The clinical management in extremely severe COPD. Respir Med 2007;101:1613-24.
Reference as: Robbins RA. COPD exacerbations: an evidence-based review. Southwest J Pulm Crit Care 2012;5:36-51. (Click here for a PDF version of the manuscript)