Claire R. Pestak, MPH 1,2
Tawny W. Boyce, MS, MPH 1
Orrin B. Myers, PhD 4
L. Olivia Hopkins, MD 3
Charles L. Wiggins, PhD 1,2,3
Bruce R. Wissore, JD, PhD, MA, MS, MS 3,6
Akshay Sood, MPH, MD 3,5
Linda S. Cook, PhD 1,3
1UNM Comprehensive Cancer Center, University of New Mexico, MSC 07-4025,
1 UNM, Albuquerque, NM, 87131, USA
2New Mexico Tumor Registry, University of New Mexico, MSC 11 6020, 1 UNM, Albuquerque, NM, 87131, USA
3Department of Internal Medicine, University of New Mexico School of Medicine, MSC 10 5550, 1 UNM, Albuquerque, NM, 87131, USA
4Department of Family and Community Medicine, University of New Mexico School of Medicine, MSC 09-5040, 1 UNM, Albuquerque, NM, 87131, USA
5Miners Colfax Medical Center, Raton, NM, 87740, USA
6Southwestern Illinois College, Belleville, IL, 62221, USA
Abstract
Background
Occupational exposures in mining and oil/gas extraction are known risk factors for thoracic malignancies (TMs). Given the relatively high proportion of these industries in New Mexico (NM), we conducted a feasibility study of adult lifetime occupational history among TM cases. We hypothesized a higher proportion of occupational TM in NM relative to the estimated national average of 10-14%.
Methods
We identified incident TM cases through the population-based New Mexico Tumor Registry (NMTR), from 2017- 2018. Cases completed a telephone interview. An adjudication panel reviewed case histories and classified cancers as probable, possible, or non-occupational related, taking into account the presence, duration, and latency of exposures. We characterized recruitment and describe job titles and exposures among those with occupational TMs. We also compared the distributions of industry between those with and without occupational TM.
Results
The NMTR identified 400 eligible TM cases, 290 of which were available to be recruited (n=285 lung/bronchial cancer; n=5 mesotheliomas). Of the latter, 60% refused and 18% were deceased, 9% had invalid addresses, 11% were unable to be reached by telephone, and 3% were too ill to participate. The 43 cases who completed an interview held 236 jobs. A total of 33% of cases were classified as probable occupational TM and 5% as possible occupational TM.
Conclusions
High rates of early mortality and refusals were significant barriers to study participation. Nonetheless, the proportion of probable occupational TMs greatly exceeded the estimated national average, highlighting the need for further study of occupational TM in the state.
Editor's Note: See The Best Laid Plans of Mice and Men for accompanying editorial.
Introduction
Lung cancer and mesothelioma are the most common thoracic malignancies (TMs). Lung cancer is the second most common cancer in the United States (US) and in New Mexico (NM) and the leading cause of cancer death (1). Mesothelioma is relatively rare but has a specific association with occupational exposure to asbestos. For this paper, lung cancer and pleural mesotheliomas are combined as TMs. Despite some treatment advances (2,3), five-year relative survival is less than 20% for all TM (4).
The strongest risk factor for lung cancer is cigarette smoking (5). Other established risk factors for TMs include exposure to asbestos, uranium, radon gas, and other cancer-causing agents in the workplace, radiation therapy to the lungs, and a family history of lung cancer (6-8). The importance of occupation in TMs is emphasized by the Global Burden of Disease (GBD) report indicating that the two main cancers caused by occupational exposures worldwide were lung cancer (274,000 deaths annually) and mesothelioma (27,000 deaths annually) (9). Various estimates attributing occupation to lung cancer include: a 1981 US estimate of 15% for men and 5% for women, or 10% overall (10), a 1987 NM estimate of 14% in men (11); and, a 2003 US estimate for deaths of 8.0%–19.2% for men and 2% for females, or 6.3%-13.0% overall (12,13). Thus we estimated that overall in the US, 10%-14% of TMs could be attributable to occupation.
Historic and current occupational exposures are of particular interest in NM. Mining, in particular uranium mining, was a major operation in NM from 1950-1970. Mining is still an important industry in this region: between 2011 and 2015, the NM mining industry saw a 20% increase in employment for all types of mining (14). NM also has significant employment in the Mining, Quarrying, and Oil and Gas Extraction industry relative to other parts of the Southwest (15). These industries have a greater share of local employment in NM than in the US overall (16). Additionally, NM was the ninth highest natural gas producer in the US in 2018, producing 1.49 million cubic feet of natural gas (17).
Given the historic and current extraction activities in NM, we hypothesized that NM would have a higher proportion of occupational TMs than the estimated national average of 10%-14%. As an initial step in estimating this occupational TM cancer burden in NM, we conducted a feasibility study to obtain adult lifetime occupational histories for TM cases.
Methods
Recruitment and Data Collection
This feasibility study was approved (#16-306) by the Human Research Review Committee at the University of New Mexico and cases provided signed, informed consent. We identified incident TM cases from February 1, 2017 to February 2, 2018 via the population-based New Mexico Tumor Registry (NMTR), a founding member of the National Cancer Institute’s (NCI) Surveillance Epidemiology and End Results (SEER) Program. Cases were identified by two methods: (1) rapid case ascertainment (RCA) via electronic pathology reports and (2) usual case ascertainment (UCA) via tumor registrars manually collecting data from around the state. Contact with eligible cases involved a three-step process. In step 1, the NMTR contacted treating physicians explaining the study and advising them of their patient’s eligibility allowing the physician to state any objection to patient contact. In step 2, the NMTR contacted the patient (letter and study brochure in English and Spanish) informing them about the study and allowing them to opt-out from further contact. In the special case of no physician of record, patients were contacted after a three month wait period. Patients who refused participation or were deceased were ineligible for study contact. In step 3, for the remainder, contact information was released to study personnel.
All potential cases in step 3 were mailed documents in both English and Spanish including: an introductory letter, a flyer about benefits counseling, a Frequently Asked Questions sheet, two copies of a Residence and Work History worksheet, a Life Events Calendar, showcards, and two copies of the consent form. One consent form was for the case to sign and keep and the other was signed and returned to the study, along with one copy of the Residence and Work History worksheet. Showcards functioned as a visual aid by listing possible answers to interview questions. The Life Events Calendar functioned as a memory aid to anchor major life events like marriages, births, deaths, relocations, job changes, and other historical events. The Residence and Work History Worksheet gave the cases a time frame to date their paid jobs and occupations, held for at least 6 months, during their adult life and was used for reference during the interview. Work did not have to occur in the state of NM. Study interviewers contacted cases by telephone to answer questions. Those who expressed a willingness to participate were asked to complete and return the worksheets/consent form and to schedule an interview.
Consenting cases completed the same structured telephone interview with an embedded script that obtained information on demographics, lifestyle factors, medical history, reproductive history (women only) and adult lifetime occupational history. For each and every job held for six months or longer from age 18 years onwards, the cases provided job title, city and country of job location, job status (full-time/part-time), job duties, exposure information on relevant agents (18) (a list of more than 30 relevant exposures was provided to cases) including the duration of each exposure, and age at start and end of the job. All cases were asked all job-related questions providing a detailed and specific work history for each individual. Data were recorded in Research Electronic Data Capture (REDCap) database (19). Cases received a small merchandise card in appreciation. All potential cases and surviving family members were given an optional referral to a benefits counselor regardless of their self-reported exposures or determination by the Data Adjudication Committee (DAC).
Determination of Occupational TM
De-identified occupational history summaries were reviewed by the DAC to determine if each case was attributable to occupational exposures, as summarized below. The DAC was composed of three voting members: a pulmonologist with expertise in occupational pulmonary diseases associated with the coal and uranium mining industries; a preventive medicine specialist with expertise in occupational health who works in the Center for Occupational Environmental Health Promotion; and, an attorney with expertise in the medicolegal definitions for causation in the occupational setting. A non-voting member (CRP) served as the committee Chair to tally votes and mediate further discussion if necessary.
This expert panel independently reviewed the de-identified individual job histories for each case, and considered exposures that had a latency of at least 10 years, exposure durations of at least one year, and exposure intensity through self-reported frequency of exposure on the job. To aid in assessment, each panel member was provided a summary table of the known strength of the association between relevant exposures and TM occurrence (available upon request) (20-27). After independent review, the panel would meet to discuss and vote on classification. If all three DAC members found sufficient evidence for relevant occupational exposure, the case was classified as a probable occupational TM. If at least one DAC member found insufficient evidence for relevant occupational exposure, the case was classified as a possible occupational TM. If all DAC members found insufficient evidence for relevant occupational exposure, the case was classified as non-occupational TM. Smoking history for each case was provided to the DAC, but occupational cancer was decided independent of smoking, except in the case of asbestos exposure where a synergistic relationship is well supported by the published literature (28). Because of the participant burden and the high likelihood of misclassification, we did not collect information on environmental tobacco smoke or biomass/coal smoke for each job reported in this study. A letter was sent to each case with the DAC’s determination.
Analysis
After the determination of occupational TM status by the DAC, each job title for each case was coded to an industry using the NIOSH Industry and Occupation Computerized Coding System (NIOCCS) (29). Each job title was submitted, and using the "Census 2010/NAICS 2007/SOC 2010" coding scheme, the most appropriate 2010 Industry Census Code provided by the industry and occupation output was selected. If the industry was unclear based on the job title alone, the work history was reviewed for the company name, job duties, or other relevant notes. In these situations, once an industry was selected, the industry was independently verified by another study team member. The possible 269 industry categories in the 2010 census system were further summarized into 20 North American Industry Classification System (NAICS) sectors (30).
Results
Of the 400 eligible cases initially identified via the NMTR, 110 (28%) were not released to study personnel for the following reasons: 33 (30%) refused to have their information released to investigators; 47 (43%) were deceased; 23 (21%) had no physician of record and were in the 3-month wait period; four (4%) had an invalid address; two (2%) were subsequently determined to be ineligible, and one case (1%) was determined to have a duplicate record in the NMTR. The remaining 290 eligible cases were invited to join the study, of which 285 had lung cancer and 5 had mesothelioma. Over-all, refusals (60%) and deaths (18%) were the two major reasons for non-participation in the interview, but cases also had invalid addresses (9%), were unable to be reached by telephone (11%), or were too ill to participate (3%). Of the 43 cases, 98% agreed to future tumor tissue testing and medical record reviews.
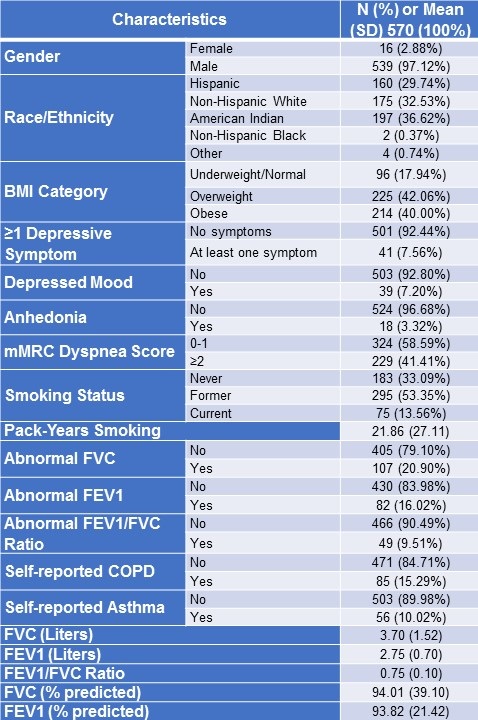
Demographic characteristics of cases are detailed in Table I.
Table I. Demographics of Thoracic Malignancies (TM) cases

Among the cases, 51% were women, 70% were Non-Hispanic White, 86% were >60 years of age, 19% reported a parent had lung cancer. In terms of insurance and benefits, 95% had some type of health insurance, but only 9% had sought compensation through Social Security Disability, Worker's Compensation, or the Veterans Administration before the study. Medical Histories of cases are detailed in Table II.
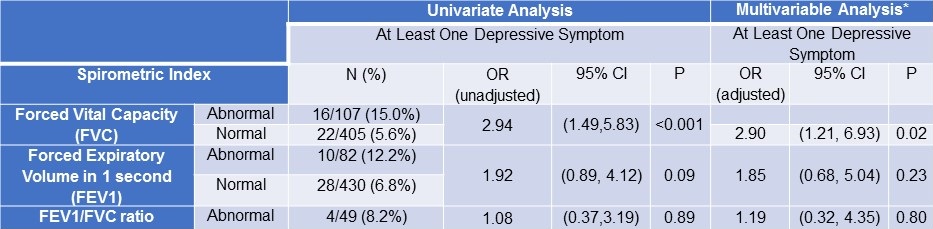
Table II. Medical History of Thoracic Malignancies (TM) cases.

Among the cases, 49% were overweight/obese. Both smoking (72% current/former cigarette smokers) and non-malignant respiratory diseases (40% reporting pulmonary fibrosis, COPD, or chronic bronchitis) were common.
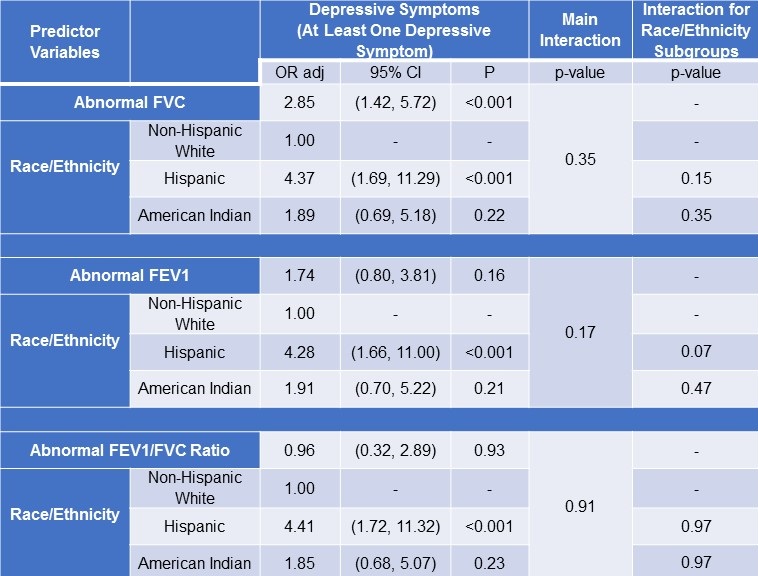
Cases reported 236 jobs representing 20 NAICS sectors, and 14 (33%) were classified as probable and 2 (5%) as possible occupational TM. Among the probable occupational TM cases, 11 (79%) were men, and both the possible occupational TMs were men. The 14 cases with a probable occupational TM self-reported one or more of the following occupational exposures: aluminum production (n=1), arsenic (n=1), asbestos (n=7), cadmium (n=1), coal-tar (n=1), diesel (n=7), ether (n=5), nickel (n=2), paint (n=1), radiation (n=1), silica (n=9), and soot (n=2). The joint distribution of these cases by job title and exposure category is shown in Figure 1.
Figure 1. Relevant Self-Reported Exposures by Job Titles per Industry Sector for the Cases with Occupationally Related Thoracic Malignancies*

*Exposures deemed to be causal by the Data Adjudication Committee.
The study population only included those who were diagnosed and captured by the NMTR from February 1, 2017 to February 2, 2018 (n=400). Case identification at the NMTR, especially for cancers like TMs where there may not be a pathology report, may be ascertained more than a year after diagnosis. A NMTR query in March 2020 for diagnoses in the same time period noted above yielded more than double the number of TM cases (n=913). Thus we had the opportunity to compare those identified early (n=400) and up to two years later (n=513) as well as those released to the study for contact (n=290) with those whose names were not released for study contact (n=110) by selected demographic and histological characteristics (Table III).
Table III. Summary of the characteristics of the lung cancer and mesothelioma cases diagnosed between 2/1/17 – 2/2/18 for the OCTOPUS Study. Data source New Mexico Tumor Registry (NMTR).

There were differences in age between the 400 cases identified during the study period (50% for those 70 years and older) and the 513 cases identified later (57% for those 70 years and older) (p<0.05) and rurality between the 400 cases identified during the study period (23% rural) and the 513 cases identified later (44% rural) (p<0.001). Apart from the obvious difference in death as this was a criteria for not releasing contact to the study, a difference in histology was noted for those released to the study (77% non-small cell carcinoma) and those not released (66% non-small cell carcinoma) (p<0.05).
Discussion
This feasibility study was designed to obtain lifetime occupational histories from a population-based sample of TM cases and to determine the proportion of such cases that were likely attributable to occupational exposures. Despite our efforts to recruit these subjects in a timely manner, high rates of early mortality and refusals were significant barriers to study enrollment, indicating that a definitive study is not possible based on these methods. Among those who participated in the study, the proportion of cases with occupational TM (33%) was two to three times higher than prevailing national estimates (10-14%). While this result is intriguing and may warrant further study, we cannot say with certainty if this result is due to the low response percentage and the possible selection bias of having cases that were more likely to have relevant occupational exposures, or if this result truly reflects the occupational exposures in NM.
Recruiting TM cases via a population-based cancer registry is challenging. In total, 25% of eligible cases died before they could be recruited to the study via the NMTR or study personnel. An even higher proportion refused, 52% of eligible cases, in part due to poor health as cancer progressed and to the burden of treatment concurrent with study participation. Such a high refusal percentage could be a source of selection bias in which various occupations were under- or over-represented, but we had no data to address this bias directly. Additionally, the study only included those who were diagnosed and captured by the NMTR from February 1, 2017 to February 2, 2018 (n=400). We noted a substantial difference in rurality between the 400 cases identified for our study (23% rural) and the 513 cases identified later (44% rural). The majority of counties in NM are rural or frontier (26/33) (31). TM cases diagnosed among residents of these areas are less likely to receive health care in facilities that are served by pathology laboratories with electronic reporting; instead cancer registrars visit the facilities to manually abstract medical records leading to a longer reporting timeline. These results imply that rural TM cases were under-represented in our study, and since those with mining and other extraction occupations are more likely to reside and get health care in rural areas, our estimate of 33% occupational TM might be an underestimate.
From the list of more than 30 possible exposures that are known or suspected carcinogens for lung cancer (32), probable occupational TM cases reported exposures to aluminum production, arsenic, asbestos, cadmium, coal-tar, diesel fumes, ether, nickel, paint, radiation, silica, and soot. Limitations of these results include the difficulty of retrospective estimation of the intensity and duration of each of these exposures at each job, and the fact that the study did not have enough cases to conduct an analysis accounting for other exposures such as tobacco use, comorbidities, and socioeconomic factors (33). Further, we did not have information on exposures to indoor smoke in the home from, for example, wood burning stoves.
The U.S. does not have a comprehensive employment and exposure database or an occupational disease mortality surveillance system that could provide more objective and comprehensive occupational information than self-report. In some countries, researchers can link data from national cancer registries and occupational databases to help confirm associations between occupational exposures and cancers (34). Inclusion of an occupational history in medical records could also provide more objective data, but such practices are currently sporadic and non-uniform. While death certificates often record a decedent’s longest or lifetime occupation, no exposure details are included, and access to this minimal data is often restricted in an effort to maintain confidentiality (35). Thus, improvements to the evaluation of occupation and occupational exposures for cancers such as TMs on a population-basis remains a challenge.
Other strengths of our study not indicated above include: our success in ascertaining a detailed adult lifetime occupational history from lung cancer survivors using an English or Spanish interview; inclusion of racial/ethnic minorities; inclusion of both men and women (with 21% of women in our study having a probable occupational TM); no eligibility restriction to a specific industry or exposure; a rigorous procedure via the DAC to establish a probable-occupational, possible-occupational, or non-occupational classification for each case; and offering cases a referral for benefits counseling (65% accepted). The limitations of this study have been discussed above.
This feasibility study suggests that 33% of cases had a probable occupational TM, two to three times the national historical estimate, highlighting the importance of exposures and jobs in the NM population that can lead to occupational TMs. However, a more definitive study is not feasible based on the methods used in this study as the ability to overcome the above-described methodological and recruitment challenges remains a significant barrier to further population-based studies of occupation-related TM in NM and the US.
Acknowledgements: This research utilized the UNM Comprehensive Cancer Center (UNMCCC) Biostatistics Shared Resource, and the UNM Clinical & Translational Science Center, the Surveillance, Epidemiology and End Results Program (SEER) data for New Mexico, and REDCap (DHHS/NIH/NCRR #8UL1TR000041).
Funding: The grant sponsor was the UNM Foundation, a non-profit corporation, organized exclusively for charitable and educational purposes under Section 501(c)(3). CRP, TWB, and LSC and the Biostatistics Shared Resource received support from the UNM Comprehensive Cancer Center (NCI P30 CA118100). CRP and CLW received support by Contract HHSN261201800014I, Task Order HHSN26100001 from the National Cancer Institute.
Institution and Ethics approval and informed consent: The work was performed at the University of New Mexico and the Human Research Review Committee (Federal wide Assurance FWA00003255) approved this study. Study participants provided written informed consent.
Acknowledgements: This research utilized the UNM Comprehensive Cancer Center (UNMCCC) Biostatistics Shared Resource, and the UNM Clinical & Translational Science Center, the Surveillance, Epidemiology and End Results Program (SEER) data for New Mexico, and REDCap (DHHS/NIH/NCRR #8UL1TR000041).
Funding: The grant sponsor was the UNM Foundation, a non-profit corporation, organized exclusively for charitable and educational purposes under Section 501(c)(3). CRP, TWB, and LSC and the Biostatistics Shared Resource received support from the UNM Comprehensive Cancer Center (NCI P30 CA118100). CRP and CLW received support by Contract HHSN261201800014I, Task Order HHSN26100001 from the National Cancer Institute.
Institution and Ethics approval and informed consent: The work was performed at the University of New Mexico and the Human Research Review Committee (Federal wide Assurance FWA00003255) approved this study. Study participants provided written informed consent.
References
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020 Jan;70(1):7-30. [CrossRef] [PubMed]
- American Cancer Society. What's new in malignant mesothelioma research? 2020 (Available from: https://www.cancer.org/cancer/malignant-mesothelioma/about/new-research.html)
- Howlader N, Forjaz G, Mooradian MJ, Meza R, Kong CY, Cronin KA, Mariotto AB, Lowy DR, Feuer EJ. The Effect of Advances in Lung-Cancer Treatment on Population Mortality. N Engl J Med. 2020 Aug 13;383(7):640-649. [CrossRef] [PubMed]
- American Cancer Society. Survival rates for mesothelioma 2020. Available at: https://www.cancer.org/cancer/malignant-mesothelioma/detection-diagnosis-staging/survival-statistics.html (accessed 1/12/21).
- Islami F, Goding Sauer A, Miller KD, Siegel RL, Fedewa SA, Jacobs EJ, McCullough ML, Patel AV, Ma J, Soerjomataram I, Flanders WD, Brawley OW, Gapstur SM, Jemal A. Proportion and number of cancer cases and deaths attributable to potentially modifiable risk factors in the United States. CA Cancer J Clin. 2018 Jan;68(1):31-54. [CrossRef] [PubMed]
- Thun MJ, Henley SJ, Travis WD. Lung cancer. In: Fraumeni Jr. JF, Schottenfeld D, editors. Cancer epidemiology and prevention. Fourth ed. New York, NY: Oxford University Press; 2018. p. 519-42.
- Ge C, Peters S, Olsson A, Portengen L, Schüz J, Almansa J, et al. Respirable Crystalline Silica Exposure, Smoking, and Lung Cancer Subtype Risks. A Pooled Analysis of Case-Control Studies. Am J Respir Crit Care Med. 2020 Aug 1;202(3):412-421. [CrossRef] [PubMed]
- Ge C, Peters S, Olsson A, Portengen L, Schuz J, Almansa J, et al. Diesel engine exhaust exposure, smoking, and lung cancer subtype risks. A pooled exposure-response analysis of 14 case-control studies. Am J Respir Crit Care Med. 2020;202(3):402-11. [CrossRef] [PubMed]
- Institute for Health Metrics and Evaluation. Global burden of disease compare viz hub Available at: https://vizhub.healthdata.org/gbd-compare/ (accessed 1/12/21).
- Doll R, Peto R. The causes of cancer: quantitative estimates of avoidable risks of cancer in the United States today. J Natl Cancer Inst. 1981 Jun;66(6):1191-308. [PubMed]
- Lerchen ML, Wiggins CL, Samet JM. Lung cancer and occupation in New Mexico. J Natl Cancer Inst. 1987 Oct;79(4):639-45. [PubMed]
- Canadian Centre for Occupational Health and Safety. Osh answers fact sheets 2017. Available at: https://www.ccohs.ca/oshanswers/diseases/occupational_cancer.html (accessed 1/12/21).
- Steenland K, Burnett C, Lalich N, Ward E, Hurrell J. Dying for work: The magnitude of US mortality from selected causes of death associated with occupation. Am J Ind Med. 2003 May;43(5):461-82. [CrossRef] [PubMed]
- New Mexico Department of Workforce Solutions. New Mexico 2017 state of the workforce report 2017. Available at: https://www.dws.state.nm.us/Portals/0/DM/LMI/NM_2017_SOTW_Report.pdf (accessed 1/12/21).
- New Mexico Department of Workforce Solutions. Industry spotlight 2013. Available at: https://www.dws.state.nm.us/Portals/0/DM/LMI/IndSpotlight_Oct2013.pdf (accesed 1/12/21).
- New Mexico Department of Workforce Solutions. New Mexico 2018 state of the workforce 2018. Avaialble at: https://www.dws.state.nm.us/Portals/0/DM/LMI/NM_2018_SOTW_Report.pdf (accessed 1/12/21).
- U.S. Energy Information Administration. Rankings: Natural gas marketed production, 2018. Available at: https://www.eia.gov/state/rankings/?sid=US#/series/47 (accessed 1/12/21).
- International Agency for Research on Cancer. IARC. Monographs on the evaluation of carcinogenic risks to humans, vol 100, a review of human carcinogens. Lyon, France: International Agency for Research on Cancer; 2011. Available from: https://publications.iarc.fr/124 (accessed 1/12/21).
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009 Apr;42(2):377-81. [CrossRef] [PubMed]
- Algranti E, Buschinelli JT, De Capitani EM. Occupational lung cancer. J Bras Pneumol. 2010 Nov-Dec;36(6):784-94. English, Portuguese. [CrossRef] [PubMed]
- Delva F, Andujar P, Lacourt A, Brochard P, Pairon JC. Facteurs de risque professionnels du cancer bronchopulmonaire [Occupational risk factors for lung cancer]. Rev Mal Respir. 2016 Jun;33(6):444-59. French. [CrossRef] [PubMed]
- Field RW, Withers BL. Occupational and environmental causes of lung cancer. Clin Chest Med. 2012 Dec;33(4):681-703. [CrossRef] [PubMed]
- Hashim D, Boffetta P. Occupational and environmental exposures and cancers in developing countries. Ann Glob Health. 2014;80(5):393-411.
- Hubaux R, Becker-Santos DD, Enfield KS, Lam S, Lam WL, Martinez VD. Arsenic, asbestos and radon: emerging players in lung tumorigenesis. Environ Health. 2012 Nov 22;11:89. [CrossRef] [PubMed]
- Peto J, Doll R, Hermon C, Binns W, Clayton R, Goffe T. Relationship of mortality to measures of environmental asbestos pollution in an asbestos textile factory. Ann Occup Hyg. 1985;29(3):305-55. [CrossRef] [PubMed]
- Rajer M, Zwitter M, Rajer B. Pollution in the working place and social status: co-factors in lung cancer carcinogenesis. Lung Cancer. 2014 Sep;85(3):346-50. [CrossRef] [PubMed]
- Steenland K, Loomis D, Shy C, Simonsen N. Review of occupational lung carcinogens. Am J Ind Med. 1996 May;29(5):474-90. [CrossRef] [PubMed]
- Klebe S, Leigh J, Henderson DW, Nurminen M. Asbestos, Smoking and Lung Cancer: An Update. Int J Environ Res Public Health. 2019 Dec 30;17(1):258. [CrossRef] [PubMed]
- U.S. Department of Health and Human Services PHS, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health, Division of Surveillance, Hazard Evaluation and Field Studies, Surveillance Branch. NIOSH industry and occupation computerized coding system (NIOCCS). 2018 (cited 2017). Available at: https://wwwn.cdc.gov/nioccs3/ (accessed 1/12/21).
- North American Industry Classification System. The National Institute for Occupational Safety and Health (NIOSH). Available at: https://www.cdc.gov/niosh/topics/coding/pdfs/Census2010CodingInstruction.pdf (accessed 1/12/21).
- Economic Research Service United States Department of Agriculture. Rural-urban continnuum codes Available at: https://www.ers.usda.gov/data-products/rural-urban-continuum-codes/ (accessed 1/12/21).
- Cogliano VJ, Baan R, Straif K, Grosse Y, Lauby-Secretan B, El Ghissassi F, et al. Preventable exposures associated with human cancers. J Natl Cancer Inst. 2011;103(24):1827-39. [CrossRef] [PubMed]
- Spyratos D, Zarogoulidis P, Porpodis K, Tsakiridis K, Machairiotis N, Katsikogiannis N, et al. Occupational exposure and lung cancer. J Thorac Dis. 2013 Sep;5 Suppl 4(Suppl 4):S440-5. [CrossRef] [PubMed]
- Pukkala E, Martinsen JI, Lynge E, Gunnarsdottir HK, Sparén P, Tryggvadottir L, Weiderpass E, Kjaerheim K. Occupation and cancer - follow-up of 15 million people in five Nordic countries. Acta Oncol. 2009;48(5):646-790. [CrossRef] [PubMed]
- National Center for Health Statistics. Restricted-use vital statistics data Available at: https://www.cdc.gov/nchs/nvss/nvss-restricted-data.htm (Accessed 1/12/21).
Cite as: Pestak CR, Boyce TW, Myers OB, Hopkins LO, Wiggins CL, Wissore BR, Sood A, Cook LS. A Population-Based Feasibility Study of Occupation and Thoracic Malignancies in New Mexico. Southwest J Pulm Crit Care. 2021;22(1):23-35. doi: https://doi.org/10.13175/swjpcc057-20 PDF
 Tuesday, June 1, 2021 at 7:00PM
Tuesday, June 1, 2021 at 7:00PM