February 2024 Medical Image of the Month: Pulmonary Alveolar Proteinosis in Myelodysplastic Syndrome
 Friday, February 2, 2024 at 8:00AM
Friday, February 2, 2024 at 8:00AM 
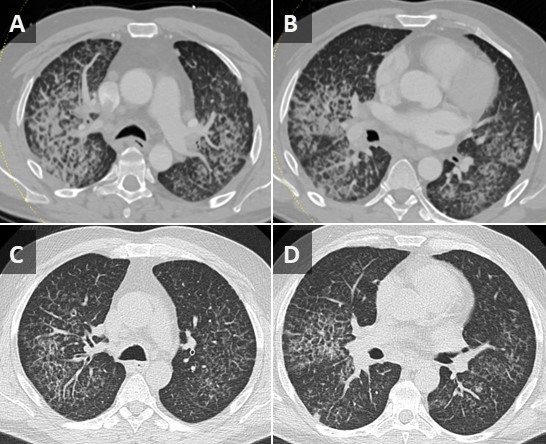
Figure 1. Axial CT images from a contrast-enhanced chest CT performed on the patient at time of admission (A,B) demonstrate a combination of smooth septal line thickening and superimposed ground glass, resulting in a “crazy paving” appearance. A noncontrast chest CT performed at an outside hospital 2 months earlier also demonstrates “crazy paving”; however, the findings have progressed significantly during the 2 intervening months.
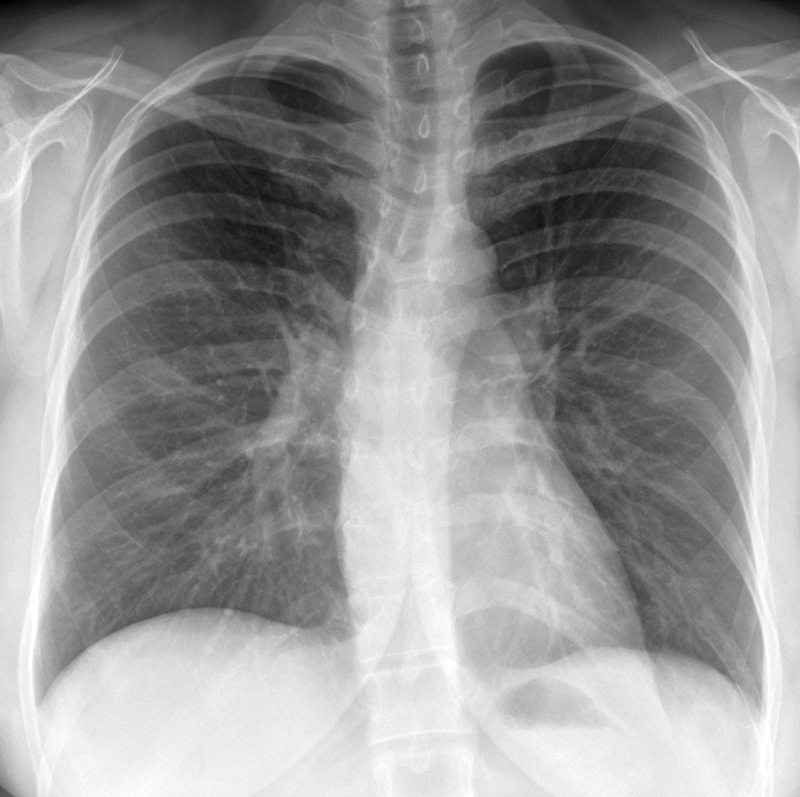
A 56-year-old man presented to our institution with weight loss, fatigue, and worsening dyspnea. A chest CT (Figure 1A,B) showed a patchy, mostly central crazy-paving pattern. An outside hospital CT performed 2 months earlier was also made available for comparison (Figure 1C,D) demonstrating interval progression of these findings. The patient also had mediastinal and hilar adenopathy. Past workup had primarily focused on the lymphadenopathy with considerations of possible lymphoma, sarcoidosis or coccidiomycosis infection. A past lymph node biopsy had revealed non-caseating granulomas and serum titers were positive for coccidiomycosis. Lymphadenopathy decreased after initiation of coccidiomycosis treatment, but symptoms and crazy paving findings continued to worsen. Further workup revealed a new diagnosis of myelodysplastic syndrome (MDS) and subsequent bronchoalveolar lavage (BAL) and histology results were consistent with secondary PAP, likely due to patient’s underlying hematologic disease.
Pulmonary alveolar proteinosis (PAP) is a rare disease characterized by the accumulation of lipoproteinaceous material in the lung alveoli. There are two types of PAP that occur in adults: Idiopathic/autoimmune and Secondary PAP. Idiopathic/autoimmune PAP is more common and is thought to result from antibody production against granulocyte-macrophage-colony-stimulating factor (GM-CSF) that regulates surfactant homeostasis. Secondary PAP results from a precipitating condition, often inhalation exposure, underlying malignancy, or immunocompromise.
The clinical manifestations of PAP are nonspecific and includes dyspnea, nonproductive cough, fatigue, and weight loss. CT may show nonspecific findings of smooth, bilateral interlobular septal thickening superimposed on a background of ground-glass opacification (crazy-paving). Diagnosis is confirmed with BAL and lung biopsy showing accumulation of eosinophilic and periodic acid-Schiff stain (PAS) positive lipoproteinaceous material within alveoli. Treatment involves pulmonary lavage for idiopathic/autoimmune PAP and treating the underlying condition for secondary PAP.
Parker Brown MD, Clint Jokerst MD, Michael Gotway MD, Matthew Stib MD
Department of Radiology
Mayo Clinic Arizona, Scottsdale, AZ
References
- Frazier AA, Franks TJ, Cooke EO, Mohammed TL, Pugatch RD, Galvin JR. From the archives of the AFIP: pulmonary alveolar proteinosis. Radiographics. 2008 May-Jun;28(3):883-99; quiz 915. [CrossRef][PubMed]
- Ioachimescu OC, Kavuru MS. Pulmonary alveolar proteinosis. Chron Respir Dis. 2006;3(3):149-59. [CrossRef] [PubMed]
- Presneill JJ, Nakata K, Inoue Y, Seymour JF. Pulmonary alveolar proteinosis. Clin Chest Med. 2004 Sep;25(3):593-613, viii. [CrossRef] [PubMed]