Ultrasound for Critical Care Physicians: Who Stole My Patient’s Trachea?
 Thursday, August 16, 2018 at 8:00PM
Thursday, August 16, 2018 at 8:00PM Monika Kakol MD, Connor Trymbulak MSc, and Rodrigo Vazquez Guillamet MD
Department of Internal Medicine Department
University of New Mexico School of Medicine
Albuquerque, NM USA
A 73-year-old man with a past medical history of asthma-chronic obstructive pulmonary disease overlap syndrome and coronary artery disease presented to the emergency department with acute on chronic respiratory failure. The patient failed to respond to initial bronchodilator treatment and non-invasive positive pressure ventilation. A decision was made to proceed with endotracheal intubation and mechanical ventilation. Upper airway ultrasonography was used to confirm positioning of the endotracheal tube and the following images were obtained:
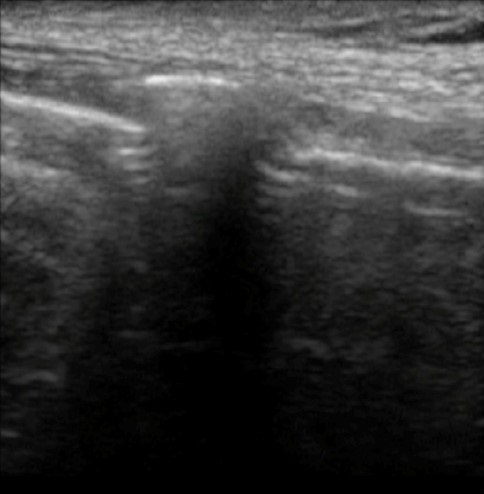
Figure 1. Longitudinal view of the trachea.

Figure 2. Transverse view of the trachea at the level of the tracheal rings.
What does the ultrasound depict (see Figures 1 & 2)? (Click on the correct answer for an explanation)
Cite as: Kakol M, Trymbulak C, Guillamet RV. Ultrasound for critical care physicians: Who stole my patient’s trachea? Southwest J Pulm Crit Care. 2018;17(2):72-5. doi: https://doi.org/10.13175/swjpcc102-18 PDF


