Comparisons between Medicare Mortality, Readmission and Complications
 Thursday, June 13, 2013 at 3:08PM
Thursday, June 13, 2013 at 3:08PM Richard A. Robbins, MD*
Richard D. Gerkin, MD ‡
*Phoenix Pulmonary and Critical Care Research and Education Foundation, Gilbert, AZ
‡Banner Good Samaritan Medical Center, Phoenix, AZ
Abstract
The Center for Medicare and Medicaid Services (CMS) has been a leading advocate of evidence-based medicine. Recently, CMS has begun adjusting payments to hospitals based on hospital readmission rates and “value-based performance” (VBP). Examination of the association of Medicare bonuses and penalties with mortality rates revealed that the hospitals with better mortality rates for heart attacks, heart failure and pneumonia had significantly greater penalties for readmission rates (p<0.0001, all comparisons). A number of specific complications listed in the CMS database were also examined for their correlations with mortality, readmission rates and Medicare bonuses and penalties. These results were inconsistent and suggest that CMS continues to rely on surrogate markers that have little or no correlation with patient-centered outcomes.
Introduction
Implementation of the Affordable Care Act (ACA) emphasized the use of evidence-based measures of care (1). However, the scientific basis for many of these performance measures and their correlation with patient-centered outcomes such as mortality, morbidity, length of stay and readmission rates have been questioned (2-6). Recently, CMS has begun adjusting payments based on readmission rates and “value-based performance” (VBP) (7). Readmission rates and complications are based on claims submitted by hospitals to Medicare (8).
We sought to examine the correlations between mortality, hospital readmission rates, complications and adjustments in Medicare reimbursement. If the system of determining Medicare reimbursements is based on achievement of better patient outcomes, then one hypothesis is that lower readmission rates would be associated with lower mortality. An additional hypothesis is that complications would be inversely associated with both mortality and readmission rates.
Methods
Hospital Compare
Data was obtained from the CMS Hospital Compare website from December 2012-January 2013 (8). The data reflects composite data of all hospitals that have submitted claims to CMS. Although a number of measures are listed, we recorded only readmissions, complications and deaths since many of the process of care measures have not been shown to correlate with improved outcomes. Patient satisfaction was not examined since higher patient satisfaction has been shown to correlate with higher admission rates to the hospital, higher overall health care expenditures, and increased mortality (9). In some instances data are presented in Hospital Compare as higher, lower or no different from the National average. In this case, scoring was done 2, 0 and 1 respectively with 0=higher, 2=lower and 1=no different.
Mortality
Mortality was obtained from Hospital Compare and is the 30-day estimates of deaths from any cause within 30 days of a hospital admission for patients hospitalized for heart attack, heart failure, or pneumonia regardless of whether the patient died while still in the hospital or after discharge. The mortality and rates are adjusted for patient characteristics including the patient’s age, gender, past medical history, and other diseases or conditions (comorbidities) the patient had at hospital arrival that are known to increase the patient’s risk of dying.
Readmission Rates
Similarly, the readmission rates are 30-day estimates of readmission for any cause to any acute care hospital within 30 days of discharge. These measures include patients who were initially hospitalized for heart attack, heart failure, and pneumonia. Similar to mortality, the readmission measures rates are adjusted for patient characteristics including the patient’s age, gender, past medical history, and other diseases or conditions (comorbidities) the patient had at hospital arrival that are known to increase the patient’s risk for readmission.
Complications
CMS calculates the rate for each complication by dividing the actual number of self-reported outcomes at each hospital by the number of eligible discharges for that measure at each hospital, multiplied by 1,000. The composite value reported on Hospital Compare is the weighted averages of the component indicators. The measures of serious complications reported are risk adjusted to account for differences in hospital patients’ characteristics. In addition, the rates reported on Hospital Compare are “smoothed” to reflect the fact that measures for small hospitals are measured less accurately (i.e., are less reliable) than for larger hospitals.
CMS calculates the hospital acquired infection data from the claims hospitals submit to Medicare. The rate for each hospital acquired infection measure is calculated by dividing the number of infections that occur within any given eligible hospital by the number of eligible Medicare discharges, multiplied by 1,000. The hospital acquired infection rates were not risk adjusted by CMS.
In addition to the composite data, individual complications listed in the CMS database were examined (Table 1).
Table 1. Complications examined that are listed in CMS data base.
|
Objects Accidentally Left in the Body After Surgery |
|
Air Bubble in the Bloodstream |
|
Mismatched Blood Types |
|
Severe Pressure Sores (Bed Sores) |
|
Falls and Injuries |
|
Blood Infection from a Catheter in a Large Vein |
|
Infection from a Urinary Catheter |
|
Signs of Uncontrolled Blood Sugar |
Medicare Bonuses and Penalties
The CMS data was obtained from Kaiser Health News which had compiled the data into an Excel database (10).
Statistical Analysis
Data was reported as mean + standard error of mean (SEM). Outcomes between hospitals rated as better were compared to those of hospitals rated as average or worse using Student’s t-test. The relationship between continuous variables was obtained using the Pearson correlation coefficient. Significance was defined as p<0.05. All p values reported are nominal, with no correction for multiple comparisons.
Results
A large database was compiled for the CMS outcomes and each of the hospital ratings (Appendix 1). There were over 2500 hospitals listed in the database.
Mortality and Readmission Rates
A positive correlation for heart attack, heart failure and pneumonia was found between hospitals with better mortality rates (p<0.001 all comparisons). In other words, hospitals with better mortality rates for heart attack tended to be better mortality performers for heart failure and pneumonia, etc. Surprisingly, the hospitals with better mortality rates for heart attack, heart failure and pneumonia had higher readmission rates for these diseases (p<0.001, all comparisons).
Examination of the association of Medicare bonuses and penalties with mortality rates revealed that the hospitals with better mortality rates for heart attacks, heart failure and pneumonia received the same compensation for value-based performance as hospitals with average or worse mortality rates (Appendix 2, p>0.05, all comparisons). However, these better hospitals had significantly larger penalties for readmission rates (Figure 1, p<0.0001, all comparisons).
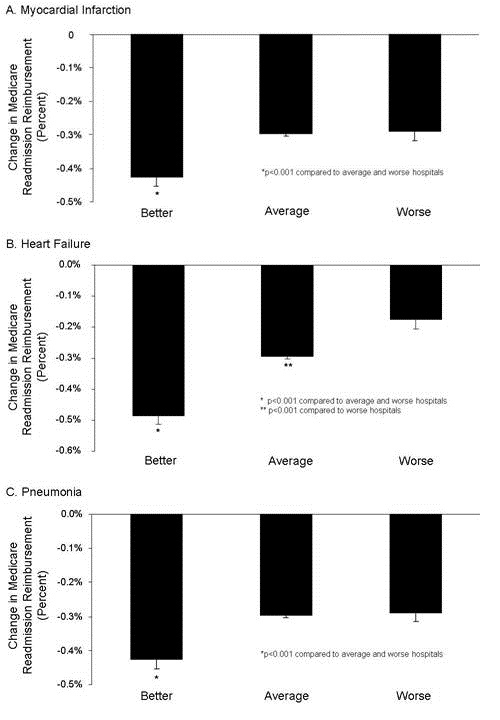
Figure 1. Medicare bonuses and penalties for readmission rates of hospitals with better, average or worse mortality for myocardial infarction (heart attack, Panel A), heart failure (Panel B), and pneumonia (Panel C).
Because total Medicare penalties are the average of the adjustment for VBP and readmission rates, the reduction in reimbursement was reflected with higher total penalty rates for hospitals with better mortality rates for heart attacks, heart failure and pneumonia (Figure 2 , p<0.001, all comparisons).
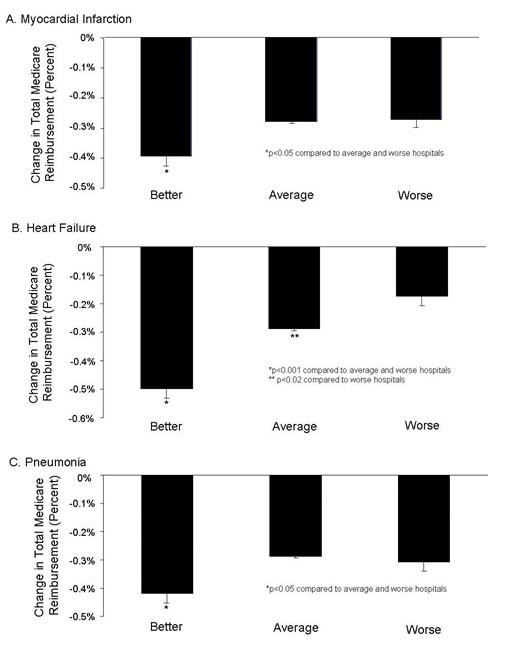
Figure 2. Total Medicare bonuses and penalties for readmission rates of hospitals with better, average or worse mortality for myocardial infarction (heart attack, Panel A), heart failure (Panel B), and pneumonia (Panel C).
Mortality Rates and Complications
The rates of a number of complications are also listed in the CMS database (Table 1). A correlation was performed for each complication compared to the hospitals with better, average or worse death and readmission rates for heart attacks, heart failure and pneumonia (Appendix 3). A positive correlation of hospitals with better mortality rates was only observed for falls and injuries in the hospitals with better death rates from heart failure (p<0.02). However, severe pressure sores also differed in the hospitals with better mortality rates for heart attack and heart failure, but this was a negative correlation (p<0.05 both comparisons). In other words, hospitals that performed better in mortality performed worse in severe pressure sores. Similarly, hospitals with better mortality rates for heart failure had higher rates of blood infection from a catheter in a large vein compared to hospitals with an average mortality rate (p<0.001). None of the remaining complications differed.
Readmission Rates and Complications
A correlation was also performed between complications and hospitals with better, average and worse readmission rates for myocardial infarction, heart failure, and pneumonia (Appendix 4). Infections from a urinary catheter and falls and injuries were more frequent in hospitals with better readmission rates for myocardial infarction, heart failure, and pneumonia compared to hospitals with the worse readmission rates (p<0.02, all comparisons). Hospitals with better readmission rates for heart failure also had higher infections from a urinary catheter compared to hospitals with average readmission rates for heart failure (p<0.001). None of the remaining complications significantly differed
Discussion
The use of “value-based performance” (VBP) has been touted as having the potential for improving care, reducing complications and saving money. However, we identified a negative correlation between deaths and readmissions, i.e., those hospitals with the better mortality rates were receiving larger financial penalties for readmissions and total compensation. Furthermore, correlations of hospitals with better mortality and readmission rates with complications were inconsistent.
Our data compliments and extends the observations of Krumholz et al. (11). These investigators examined the CMS database from 2005-8 for the correlation between mortality and readmissions. They identified an inverse correlation between mortality and readmission rates with heart failure but not heart attacks or pneumonia. However, with the financial penalties now in place for readmissions, it now seems likely hospital practices may have changed.
CMS compensating hospitals for lower readmission rates is disturbing since higher readmission rates correlated with better mortality. This equates to rewarding hospitals for practices leading to lower readmission rates but increase mortality. The lack of correlation for the other half of the payment adjustment, so called “value-based purchasing” is equally disturbing since if apparently has little correlation with patient outcomes.
Although there is an inverse correlation between mortality and readmissions, this does not prove cause and effect. The causes of the inverse association between readmissions and mortality rates are unclear, but the most obvious would be that readmissions may benefit patient survival. The reason for the lack of correlation between mortality and readmission rates with most complication rates is also unclear. VBP appears to rely heavily on complications that are generally infrequent and in some cases may be inconsequential. Furthermore, many of the complications are for all intents and purposes self-reported by the hospitals to CMS since they are based on claims data. However, the accuracy of these data has been called into question (12,13). Meddings et al. (13) studied urinary tract infections. According to Meddings, the data were “inaccurate” and not were “not valid data sets for comparing hospital acquired catheter-associated urinary tract infection rates for the purpose of public reporting or imposing financial incentives or penalties”. The authors proposed that the nonpayment by Medicare for “reasonably preventable” hospital-acquired complications resulted in this discrepancy. Inaccurate data may lead to the lack of correlation a complication and outcomes on the CMS database.
According to the CMS website the complications were chosen by “wide agreement from CMS, the hospital industry and public sector stakeholders such as The Joint Commission (TJC) , the National Quality Forum (NQF), and the Agency for Healthcare Research and Quality (AHRQ) , and hospital industry leaders” (7). However, some complications such as air bubble in the bloodstream or mismatched blood types are quite rare. Others such as signs of uncontrolled blood sugar are not evidence-based (14). Other complications actually correlated with improved mortality or readmission rates. It seems likely that some of the complications might represent more aggressive treatment or could reflect increased clinical care staffing which has previously been associated with better survival (14,15).
There are several limitations to our data. First and foremost, the data are derived from CMS Hospital Compare where the data has been self-reported by hospitals. The validity and accuracy of the data has been called into question (12,13). Second, data are missing in multiple instances. For example, data from Maryland were not present. There were multiple instances when the data were “unavailable” or the “number of cases are too small”. Third, in some instances CMS did not report actual data but only higher, lower or no different from the National average. Fourth, much of the data are from surrogate markers, a fact which is puzzling when patient-centered outcomes are available. In addition, some of these surrogate markers have not been shown to correlate with outcomes.
It is unclear if CMS Hospital Compare should be used by patients or healthcare providers when choosing a hospital. At present it would appear that the dizzying array of data reported overrelies on surrogate markers which are possibly inaccurate. Lack of adequate outcomes data and even obfuscating the data by reporting the data as average, below or above average does little to help shareholders interpret the data. The failure to apparently incorporate mortality rates as a component of VBP is another major limitation. The accuracy of the data is also unclear. Until these shortcomings can be improved, we cannot recommend the use of Hospital Compare by patients or providers.
References
- Obama B. Securing the future of American health care. N Engl J Med. 2012; 367:1377-81.
- Showalter JW, Rafferty CM, Swallow NA, Dasilva KO, Chuang CH. Effect of standardized electronic discharge instructions on post-discharge hospital utilization. J Gen Intern Med. 2011;26(7):718-23.
- Heidenreich PA, Hernandez AF, Yancy CW, Liang L, Peterson ED, Fonarow GC. Get With The Guidelines program participation, process of care, and outcome for Medicare patients hospitalized with heart failure. Circ Cardiovasc Qual Outcomes. 2012 ;5(1):37-43.
- Hurley J, Garciaorr R, Luedy H, Jivcu C, Wissa E, Jewell J, Whiting T, Gerkin R, Singarajah CU, Robbins RA. Correlation of compliance with central line associated blood stream infection guidelines and outcomes: a review of the evidence. Southwest J Pulm Crit Care. 2012;4:163-73.
- Robbins RA, Gerkin R, Singarajah CU. Relationship between the Veterans Healthcare Administration Hospital Performance Measures and Outcomes. Southwest J Pulm Crit Care 2011;3:92-133.
- Padrnos L, Bui T, Pattee JJ, Whitmore EJ, Iqbal M, Lee S, Singarajah CU, Robbins RA. Analysis of overall level of evidence behind the Institute of Healthcare Improvement ventilator-associated pneumonia guidelines. Southwest J Pulm Crit Care. 2011;3:40-8.
- http://www.medicare.gov/HospitalCompare/Data/linking-quality-to-payment.aspx (accessed 4/8/13).
- http://www.medicare.gov/hospitalcompare/ (accessed 4/8/13).
- Fenton JJ, Jerant AF, Bertakis KD, Franks P. The cost of satisfaction: a national study of patient satisfaction, health care utilization, expenditures, and mortality. Arch Intern Med. 2012;172:405-11.
- http://capsules.kaiserhealthnews.org/wp-content/uploads/2012/12/Value-Based-Purchasing-And-Readmissions-KHN.csv (accessed 4/8/13).
- Krumholz HM, Lin Z, Keenan PS, Chen J, Ross JS, Drye EE, Bernheim SM, Wang Y, Bradley EH, Han LF, Normand SL. Relationship between hospital readmission and mortality rates for patients hospitalized with acute myocardial infarction, heart failure, or pneumonia. JAMA. 2013;309(6):587-93. doi: 10.1001/jama.2013.333.
- Robbins RA. The emperor has no clothes: the accuracy of hospital performance data. Southwest J Pulm Crit Care. 2012;5:203-5.
- Meddings JA, Reichert H, Rogers MA, Saint S, Stephansky J, McMahon LF. Effect of nonpayment for hospital-acquired, catheter-associated urinary tract infection: a statewide analysis. Ann Intern Med. 2012;157:305-12.
- NICE-SUGAR Study Investigators. Intensive versus conventional insulin therapy in critically ill patients. N Engl J Med. 2009;360:1283-97.
- Robbins RA, Gerkin R, Singarajah CU. Correlation between patient outcomes and clinical costs in the va healthcare system. Southwest J Pulm Crit Care. 2012;4:94-100.
Reference as: Robbins RA, Gerkin RD. Comparisons between Medicare mortality, morbidity, readmission and complications. Southwest J Pulm Crit Care. 2013;6(6):278-86. PDF
