Correlation between Patient Outcomes and Clinical Costs in the VA Healthcare System
 Friday, April 6, 2012 at 8:26AM
Friday, April 6, 2012 at 8:26AM Richard A. Robbins, M.D.1
Richard Gerkin, M.D.2
Clement U. Singarajah, M.D.1
1Phoenix Pulmonary and Critical Care Medicine Research and Education Foundation and 2Banner Good Samaritan Medical Center, Phoenix, AZ
Abstract
Introduction: Increased nursing staffing levels have previously been associated with improved patient outcomes. However, the effects of physician staffing and other clinical care costs on clinical outcomes are unknown.
Methods: Databases from the Department of Veterans Affairs were searched for clinical outcome data including 30-day standardized mortality rate (SMR), observed minus expected length of stay (OMELOS) and readmission rate. These were correlated with costs including total, drug, lab, radiology, physician (MD), and registered nurse (RN), other clinical personnel costs and non-direct care costs.
Results: Relevant data were obtained from 105 medical centers. Higher total costs correlated with lower intensive care unit (ICU) SMR (r=-0.2779, p<0.05) but not acute care (hospital) SMR. Higher costs for lab, radiology, MD and other direct care staff costs and total direct care costs correlated with lower ICU and acute care SMR (p<0.05, all comparisons). Higher RN costs correlated only with ICU SMR. None of the clinical care costs correlated with ICU or acute care OMELOS with the exception of higher MD costs correlating with longer OMELOS. Higher clinical costs correlated with higher readmission rates (p<0.05, all comparisons). Nonclinical care costs (total costs minus direct clinical care costs) did not correlate with any outcome.
Conclusions: Monies spent on clinical care generally improve SMR. Monies spent on nonclinical care generally do not correlate with outcomes.
Introduction
Previous studies have demonstrated that decreased nurse staffing adversely affects patient outcomes including mortality in some studies (1-5). However, these studies have been criticized because studies are typically cross-sectional in design and do not account for differences in patients’ requirements for nursing care. Other observers have asked whether differences in mortality are linked not to nursing but to unmeasured variables correlated with nurse staffing (6-9). In this context, we correlate mortality with costs associated with other clinical expenditures including drug, lab, radiology, physician (MD), and other clinical personnel costs.
The observed minus the expected length of stay (OMELOS) and readmission rates are two outcome measures that are thought to measure quality of care. It is often assumed that increased OMELOS or readmission rates are associated with increased expenditures (10,11). However, data demonstrating this association are scant. Therefore, we also examined clinical care costs with OMELOS and readmission rates.
Methods
The study was approved by the Western IRB.
Hospital level of care. For descriptive purposes, hospitals were grouped into levels of care. These are classified into 4 levels: highly complex (level 1); complex (level 2); moderate (level 3), and basic (level 4). In general, level 1 facilities and some level 2 facilities represent large urban, academic teaching medical centers.
Clinical outcomes. SMR and OMELOS were obtained from the Inpatient Evaluation Center (IPEC) for fiscal year 2009 (12). Because this is a restricted website, the data for publication were obtained by a Freedom of Information Act (FOIA) request. SMR was calculated as the observed number of patients admitted to an acute care ward or ICU who died within 30 days divided by the number of predicted deaths for the acute care ward or ICU. Admissions to a VA nursing home, rehabilitation or psychiatry ward were excluded. Observed minus expected length of stay (OMELOS) was determined by subtracting the observed length of stay minus the predicted length of stay for the acute care ward or ICU from the risk adjusted length of stay model (12). Readmission rate was expressed as a percentage of patients readmitted within 30 days.
Financial data. Financial data were obtained from the VSSC menu formerly known as the klf menu. Because this is also a restricted website, the data for publication were also obtained by a Freedom of Information Act (FOIA) request. In each case, data were expressed as costs per unique in order to compare expenditures between groups. MD and RN costs reported on the VSSC menu were not expressed per unique but only per full time equivalent employee (FTE). To convert to MD or RN cost per unique, the costs per FTE were converted to MD or RN cost per unique as below (MD illustrated):
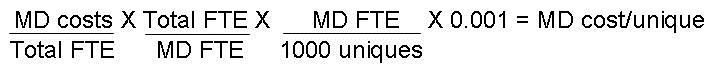
Similarly, all other direct care personnel costs/unique was calculated as below:
Direct care costs were calculated as the sum of drug, lab, x-ray, MD, RN, and other direct care personnel costs. Non-direct care costs were calculated as total costs minus direct care costs.
Correlation of Outcomes with Costs. Pearson correlation coefficient was used to determine the relationship between outcomes and costs. Significance was defined as p<0.05.
Results
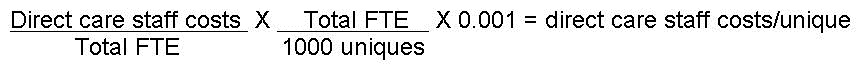
Costs: The average cost per unique was $6058. Direct care costs accounted for 53% of the costs while non-direct costs accounted for 47% of the costs (Table 1 and Appendix 1).
Table 1. Average and percent of total costs/unique.
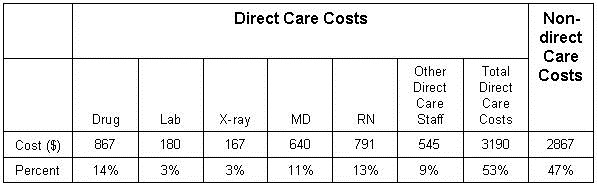
Hospital level. Data were available from 105 VA medical centers with acute care wards and 98 with ICUs. Consistent with previous data showing improved outcomes with larger medical centers, hospitals with higher levels of care (i.e. hospitals with lower level numbers) had decreased ICU SMR (Table 2). Higher levels of care also correlated with decreased ICU OMELOS and readmission rates (Table 2). For full data and other correlations see Appendix 1.
Table 2. Hospital level of care compared to outcomes. Lower hospital level numbers represent hospitals with higher levels of care.
*p<0.05
SMR. Increased total costs correlated with decreased intensive care unit (ICU) SMR (Table 3, r=-0.2779, p<0.05) but not acute care (hospital) SMR. Increased costs for lab, radiology, MD and other direct care staff costs and total direct care costs also correlated with decreased SMR for both ICU and acute care SMR (p<0.05, all comparisons). However, drug costs did not correlate with either acute care or ICU SMR. Increased RN costs correlated with improved ICU SMR but not acute care SMR. For full data and other correlations see Appendix 1.
Table 3. Correlation of SMR and costs.
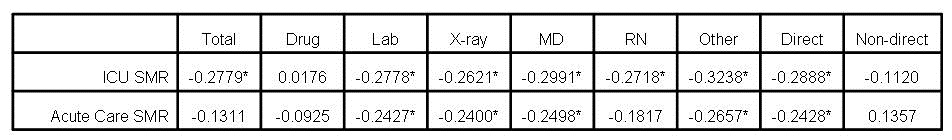
*p<0.05
OMELOS. There was no correlation between SMR and OMELOS for either acute care (r= -0.0670) or ICU (r= -0.1553). There was no correlation between acute care or ICU OMELOS and clinical expenditures other than higher MD costs positively correlated with increased OMELOS (Table 4, p<0.05, both comparisons).
Table 4. Correlation of OMELOS and costs
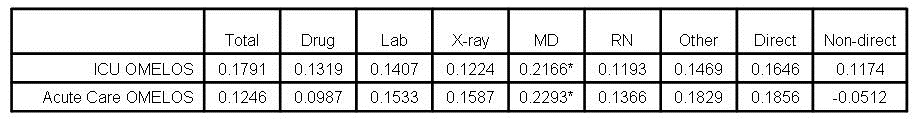
*p<0.05
Readmission rate. There was no correlation between readmission rates and acute care SMR (r= -0.0074) or ICU SMR (r= 0.0463).Total and all clinical care costs directly correlated with readmission rates while non-direct clinical care costs did not (Table 5).
Table 5.Correlation of readmission rates and costs.
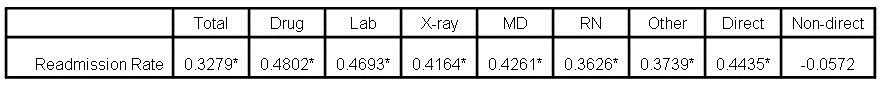
*p<0.05
Discussion
The data in this manuscript demonstrate that most clinical costs are correlated with a decreased or improved SMR Only MD costs correlate with OMELOS but all clinical costs directly correlate with increased readmission rates. However, non-direct care costs do not correlate with any clinical outcome.
A number of studies have examined nurse staffing. Increased nurse staffing levels are associated with improved outcomes, including mortality in some studies (1-5). The data in the present manuscript confirm those observations in the ICU but not for acute care (hospital). However, these data also demonstrate that higher lab, X-ray and MD costs also correlate with improved SMR. Interestingly, the strongest correlation with both acute care and ICU mortality was MD costs. We speculate that these observations are potentially explained that with rare exception, nearly all physicians see patients in the VA system. The same is not true for nurses. A number of nurses are employed in non-patient care roles such as administration, billing, quality assurance, etc. It is unclear to what extent nurses without patient care responsibilities were included in the RN costs.
These data support that readmission rates are associated with higher costs but do not support that increased OMELOS is associated with higher costs implying that efforts to decrease OMELOS may be largely wasted since they do not correlate with costs or mortality. It is unclear whether the increased costs with readmissions are because readmissions lead to higher costs or the higher clinical care costs cause the higher readmissions, although the former seem more likely.
These data are derived from the VA, the Nation’s largest healthcare system. The VA system has unique features and actual amounts spent on direct and non-direct clinical care may differ from other healthcare systems. There may be aspects of administrative costs that are unique to the VA system, although it is very likely there is applicability of these findings to other healthcare systems.
A major weakness of these data is that it is self reported. Data reported to central reporting agencies may be confusing with overlapping cost centers. Furthermore, personnel or other costs might be assigned to inappropriate cost centers in order to meet certain administrative goals. For example, 5 nurses and 1 PhD scientist were assigned to the pulmonary clinic at the Phoenix VA Medical Center while none performed any services in that clinic (Robbins RA, unpublished observations). These types of errors could lead to inaccurate or inappropriate conclusions after data analysis.
A second weakness is that the observational data reported in this manuscript are analyzed by correlation. Correlation of decreased clinical care spending with increased mortality does not necessarily imply causation (13). For example, clinical costs are increased with readmission rates. However, readmission rates may also be higher with sicker patients who require readmission more frequently. The increased costs could simply represent the higher costs of caring for sicker patients.
A third weakness is that non-direct care costs are poorly defined by these databases. These costs likely include such essential services as support service personnel, building maintenance, food preparation, utilities, etc. but also include administrative costs. Which of these services account for variation in non-direct clinical costs is unknown. However, administrative efficiency is known to be poor and declining in the US, with increasing numbers of administrators leading to increasing administrative costs (14).
A number of strategies to control medical expenditures have been initiated, although these have almost invariably been directed at clinical costs. Programs designed to limit clinical expenditures such as utilization reviews of lab or X-ray expenditures or decreasing clinical MD or RN personnel have become frequent. Even if costs are reduced, the present data imply that these programs may adversely affect patient mortality, suggesting that caution in limiting clinical expenses are needed. In addition, programs have been initiated to reduce both OMELOS and readmission rates. Since neither costs nor mortality correlate with OMELOS, these data imply that programs focusing on reducing OMELOS are unlikely to be successful in improving mortality or in reducing costs.
Non-direct patient care costs accounted for nearly half of the total healthcare costs in this study. It is unknown which cost centers account for variability in non-clinical areas. Since non-direct care costs do not correlate with outcomes, focus on administrative efficiency could be a reasonable performance measure to reduce costs. Such a performance measure has been developed by the Inpatient and Evaluation Center at the VA (15). This or similar measures should be available to policymakers to provide better care at lower costs and to incentivize administrators to adopt practices that lead to increased efficiency.
References
- Needleman J, Buerhaus P, Mattke S, Stewart M, Zelevinsky K. Nurse-staffing levels and the quality of care in hospitals. N Engl J Med 2002;346:1715-22.
- Aiken LH, Clarke SP, Sloane DM, Sochalski J, Silber JH. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA 2002;288:1987-93.
- Aiken LH, Cimiotti JP, Sloane DM, Smith HL, Flynn L, Neff DF. Effects of nurse staffing and nurse education on patient deaths in hospitals with different nurse work environments. Med Care 2011;49:1047-53.
- Diya L, Van den Heede K, Sermeus W, Lesaffre E. The relationship between in-hospital mortality, readmission into the intensive care nursing unit and/or operating theatre and nurse staffing levels. J Adv Nurs 2011 Aug 25. doi: 10.1111/j.1365-2648.2011.05812.x. [Epub ahead of print]
- Cho SH, Hwang JH, Kim J. Nurse staffing and patient mortality in intensive care units. Nurs Res 2008;57:322-30.
- Volpp KG, Rosen AK, Rosenbaum PR, Romano PS, Even-Shoshan O, Canamucio A, Bellini L, Behringer T, Silber JH. Mortality among patients in VA hospitals in the first 2 years following ACGME resident duty hour reform. JAMA 2007;298:984-92.
- Lagu T, Rothberg MB, Nathanson BH, Pekow PS, Steingrub JS, Lindenauer PK. The relationship between hospital spending and mortality in patients with sepsis. Arch Intern Med 2011;171:292-9.
- Cleverley WO, Cleverley JO. Is there a cost associated with higher quality? Healthc Financ Manage 2011;65:96-102.
- Chen LM, Jha AK, Guterman S, Ridgway AB, Orav EJ, Epstein AM. Hospital cost of care, quality of care, and readmission rates: penny wise and pound foolish? Arch Intern Med 2010;170:340-6.
- Render ML, Almenoff P. The veterans health affairs experience in measuring and reporting inpatient mortality. In Mortality Measurement. February 2009. Agency for Healthcare Research and Quality, Rockville, MD. http://www.ahrq.gov/qual/mortality/VAMort.htm
- Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med;360:1418-28.
- Render ML, Kim HM, Deddens J, Sivaganesin S, Welsh DE, Bickel K, Freyberg R, Timmons S, Johnston J, Connors AF Jr, Wagner D, Hofer TP. Variation in outcomes in Veterans Affairs intensive care units with a computerized severity measure. Crit Care Med 2005;33:930-9.
- Aldrich J. Correlations genuine and spurious in Pearson and Yule. Statistical Science 1995;10:364-76.
- Woolhandler S, Campbell T, Himmelstein DU. Health care administration in the United States and Canada: micromanagement, macro costs. Int J Health Serv. 2004;34:65-78.
- Gao J, Moran E, Almenoff PL, Render ML, Campbell J, Jha AK. Variations in efficiency and the relationship to quality of care in the Veterans health system. Health Aff (Millwood) 2011;30:655-63.
Click here for Appendix 1.
Reference as: Robbins RA, Gerkin R, Singarajah CU. Correlation between patient outcomes and clinical costs in the va healthcare system. Southwest J Pulm Crit Care 2012;4:94-100. (Click here for a PDF version)
